Overview of Opioid Treatment Program Regulations by State
Restrictive rules put evidence-based medication treatment out of reach for many

Overview
Opioid treatment programs (OTPs) are the only health care facilities that can offer patients all three forms of FDA-approved medication for opioid use disorder (OUD): methadone, buprenorphine, and injectable extended-release naltrexone.1 But Pew found that nearly all states have rules governing OTPs that are not based in evidence and in turn limit access to care or worsen patient experience.2
These rules governing the establishment, operation, and provision of care at OTPs exist at both the federal and state levels: The federal government establishes baseline requirements for OTPs, and states layer additional requirements on top of them.3 Although debate over the future of federal methadone regulation is ongoing, state policymakers have the opportunity to act now to improve access to this medication and the quality of OTP services, as well as remove rules that go beyond federal restrictions and limit access to care.4
This chartbook examines OTP regulations across all 50 states and the District of Columbia as of June 2021 in two areas:
Access to care: Regulations that affect the ease with which patients access care at OTPs, such as dictating whether one is located close to where they live or work, whether services are available at convenient times, or whether patients must obtain a government ID to start treatment.
Patient experience: Rules that affect how patients receive care, such as whether they receive medication to take at home or if they have to go to the clinic every day. State regulations can help or hinder access to high-quality, evidence-based care that is aligned with federal rules and tailored to meet patients’ needs.
Methadone is offered only in OTPs, which is one reason they are critical to reducing overdose deaths and providing lifesaving addiction treatment. State policymakers should review these rules and, where needed, revise them so that residents with OUD can access high-quality, lifesaving treatment.
Access to care
OTPs are not available in many communities. As of 2018, 80% of counties in the U.S., representing nearly a quarter of the population, had no OTPs.5 Even when a facility is nearby, patients may have challenges accessing care if services aren’t available at convenient times or patients must show a government ID to receive methadone.
How states choose to regulate OTPs plays a role in how great these access challenges are.
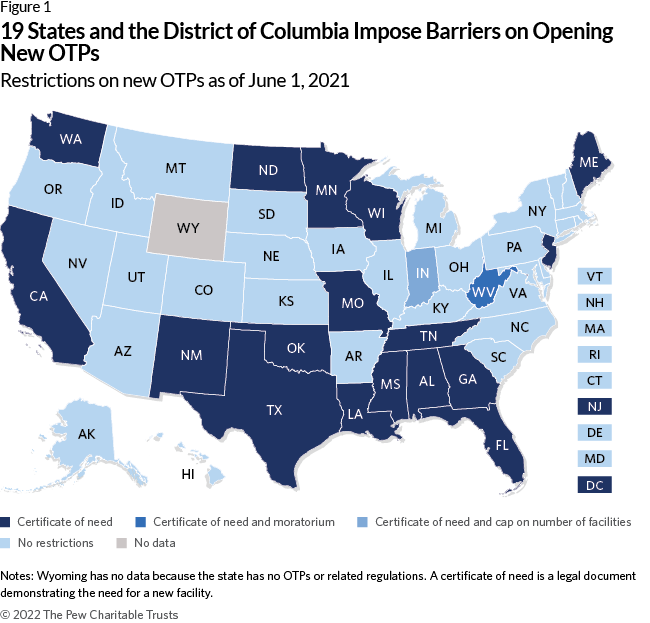
Restrictions on new OTPs
Nineteen states and the District of Columbia restrict providers from opening new OTPs in some way:
All 20 require a certificate of need, a legal document demonstrating that there is a need for a new facility. And Indiana limits the number of new facilities that can open.
West Virginia is the most restrictive state, with a legal moratorium disallowing new OTPs.
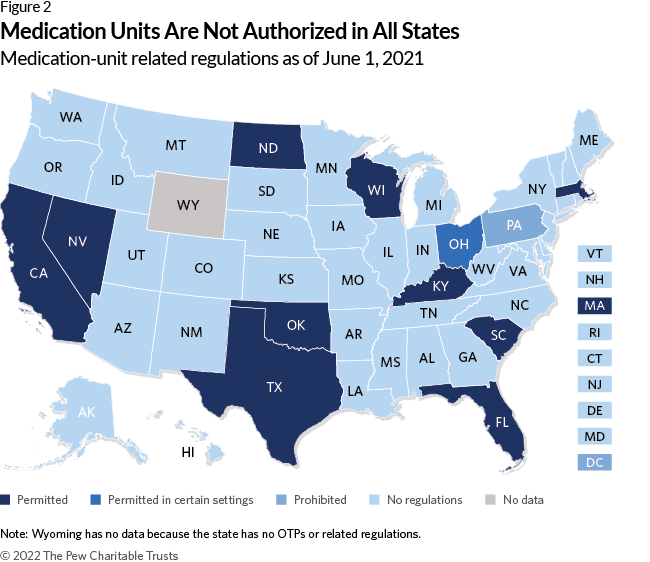
Medication units
Conversely, allowing OTPs to open medication units—locations that may offer dosing and urine screens and are affiliated with an existing OTP—can make treatment more convenient for patients who receive methadone by expanding the locations where they can receive care.6
Eleven states explicitly permit medication units, while one— Pennsylvania—prohibits them. Ohio specifically allows medication units to operate in homeless shelters, jails, prisons, local boards of public health, community health centers, residential treatment providers, small counties, and counties in Appalachia.7
Pharmacy-related barriers
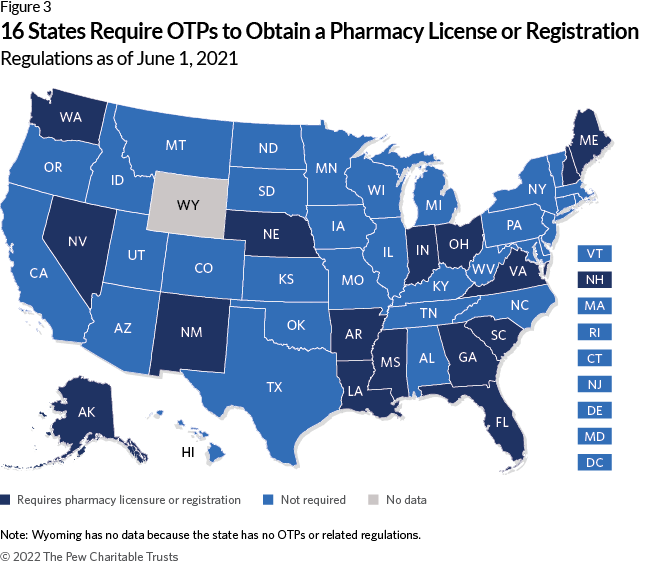
Requiring pharmacy licensure or registration
Another barrier to establishing new OTPs mandates that they be licensed or registered as pharmacies.
This is not required by federal law.8 Sixteen states have these rules.
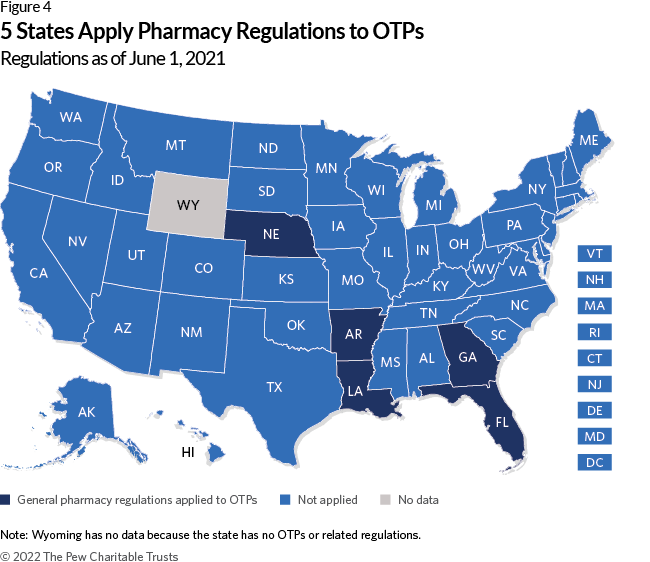
Applying general pharmacy regulations to OTPs
States that require OTPs to follow their general pharmacy regulations— which apply to a neighborhood drugstore that fills prescriptions for many medications that are used for multiple conditions—make establishing new OTPs even more challenging.
Five states apply general pharmacy regulations to OTPs.
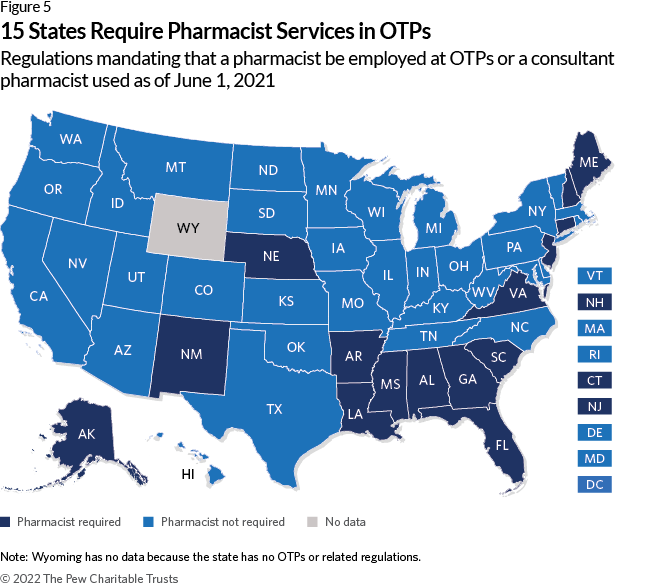
Requiring pharmacist services
Federal law allows methadone administration by a variety of licensed health care professionals including registered nurses, licensed practical nurses, or other health care professionals who are otherwise authorized to dispense opioids.9
However, 15 states require OTPs to hire a pharmacist or a consultant pharmacist, who provides guidance on the appropriateness and safety of medication use.10
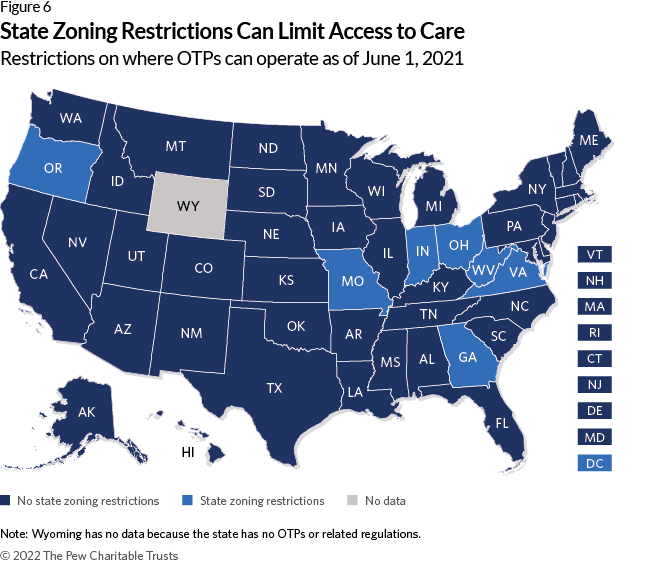
Zoning
State zoning restrictions
Restrictions on where an OTP can operate, beyond those that apply to other medical facilities, is not considered to be best practice.11
Seven states and the District of Columbia have these rules. However, in the District, the regulation supports access to care because OTPs are required to be located near public transportation.
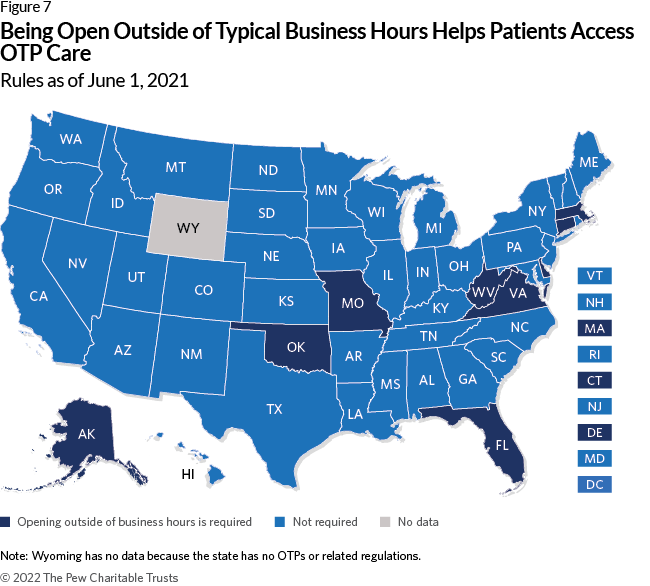
Hours of operation
Requiring OTPs to be open outside of regular business hours (e.g., outside of 8 a.m.-5 p.m.) provides flexibility for clients who may find it difficult to go to the clinic each day due to other responsibilities such as work or family obligations.12
Nine states require OTPs to be open outside of business hours.
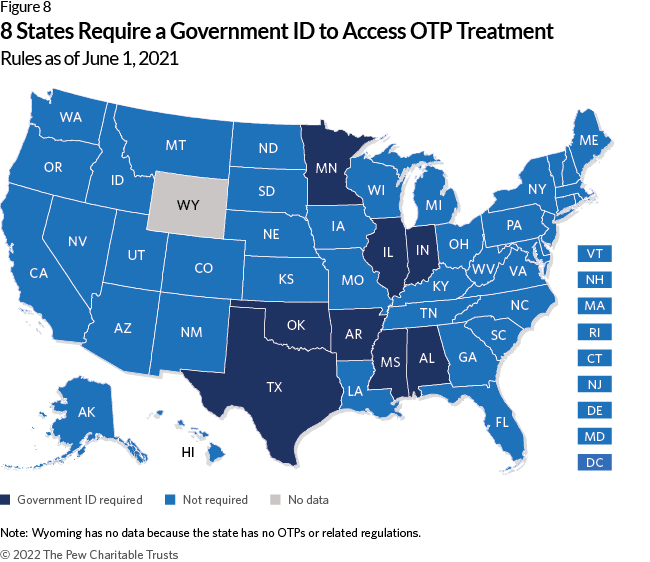
Government ID
Some people—including undocumented immigrants, people who have been incarcerated, people experiencing homelessness, and many other populations— face challenges in obtaining an ID.13 Requiring a client to show government ID to be admitted to an OTP can be a barrier to care.
Eight states have this requirement.
Conversely, California allows OTPs to provide patient identification cards that include the individual’s photo, a unique identifier, and a physical description.14 This allows the OTP to verify the patient’s identity before dispensing methadone without requiring a government ID.
Patient experience
Federal rules already dictate the frequency of urine drug screens and whether patients can receive take-home methadone—a supply of medication for opioid use disorder that allows patients to avoid having to go to the clinic each day—as well as other aspects of OTP care.
When states add additional rules, they further constrain providers from offering individualized, high-quality care that meets their patients’ needs.
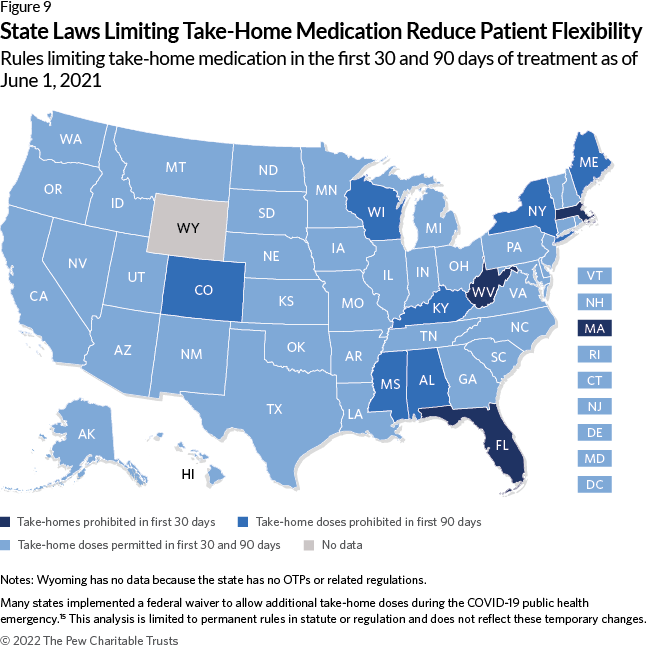
Eligibility for take-home doses
Before the COVID-19 public health emergency, federal rules allowed a single take-home dose per week in the first 90 days of treatment if patients met specific stability criteria.16 This requirement has not been permanently changed, and only temporary flexibilities have been granted as of April 2022.17
Ten states go beyond federal rules by prohibiting take-home doses in the first 30 days of treatment. Of these, seven states prohibit this practice during the full first 90 days of care.
Additional stability criteria
Federal rules require that patients meet eight stability criteria to receive take-home doses:
- Absence of recent abuse of drugs (opioid or non-narcotic), including alcohol.
- Regularity of clinic attendance.
- Absence of serious behavioral problems at the clinic.
- Absence of known recent criminal activity, e.g., drug dealing.
- Stability of the patient’s home environment and social relationships.
- Length of time in comprehensive maintenance treatment.
- Assurance that take-home medication can be safely stored within the patient’s home.
- Whether the rehabilitative benefit the patient derived from decreasing the frequency of clinic attendance outweighs the potential risks of diversion.18
Ten states impose additional stability criteria. For example, Missouri also requires that patients “demonstrate a level of stability as evidenced by … employment, actively seeking employment, or attending school if not retired, disabled, functioning as a homemaker, or otherwise economically stable.”19
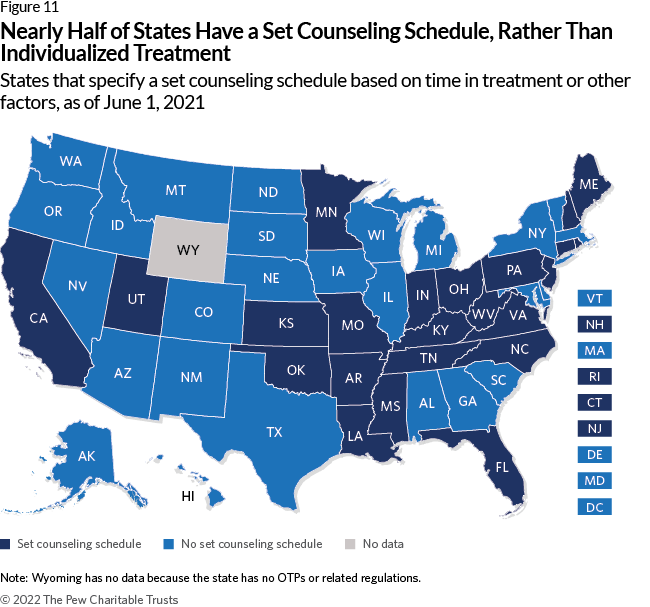
Inflexible counseling requirements
Requiring clients to participate in a set counseling schedule (e.g., a minimum number or length of sessions) to stay in treatment or receive take-home medication is not in line with federal regulations, and strict counseling requirements can reduce retention in treatment.20
Twenty-three states impose a set counseling schedule. These rules can be tied to eligibility for take-home medication. In Oklahoma, for example, patients move through five phases of treatment based on time in treatment and compliance with program rules, including participation in a set number of individual and group counseling sessions per phase. Each phase provides more take-home doses.21
These rules are not aligned with evidence, which shows that medication for opioid use disorder can be effective without counseling.22
Forcing people to leave treatment for violating program rules
It’s common for people who use opioids to also use multiple substances as well as return to opioid use, even among people on medications for opioid use disorder (MOUD).23 Although federal guidelines and recommendations list neither as a reason to end medication treatment and research supports that continuing MOUD is safer than suddenly stopping treatment, some programs “administratively discharge”—or terminate—clients because of continued drug use.24
Only Massachusetts and South Dakota prohibit administrative discharge for not being abstinent.
All states allow administrative discharge for missed methadone doses, although federal guidelines recommend reassessing patients who miss more than four methadone doses rather than terminating their treatment.25
All states also allow administrative discharge for nonparticipation in counseling or other ancillary services, even though the American Society of Addiction Medicine says the decision to decline these services should not affect a patient’s ability to obtain MOUD.26
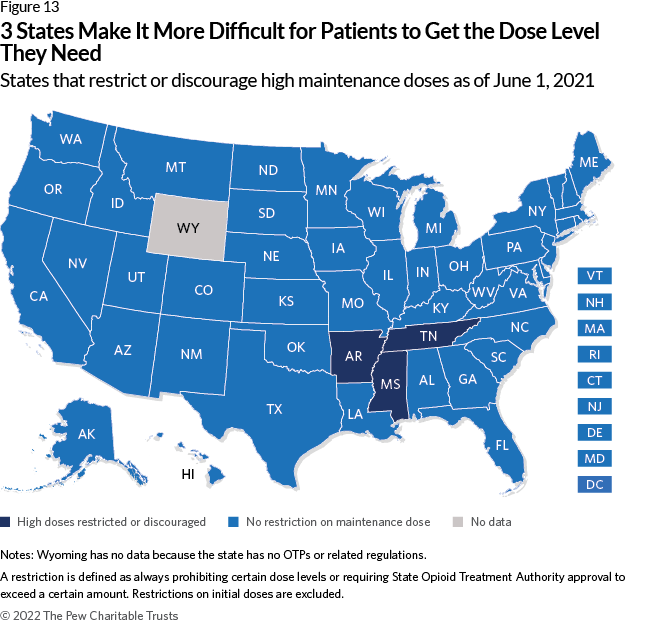
Restricting medication dosage
Doses that are too low may not effectively reduce drug cravings or use.27 Restricting or discouraging higher doses of medication may cause patients to discontinue treatment. This restriction is also not aligned with federal guidelines or evidence, as higher doses can lead to greater reductions in drug use among patients with OUD.28
Three states have these rules.
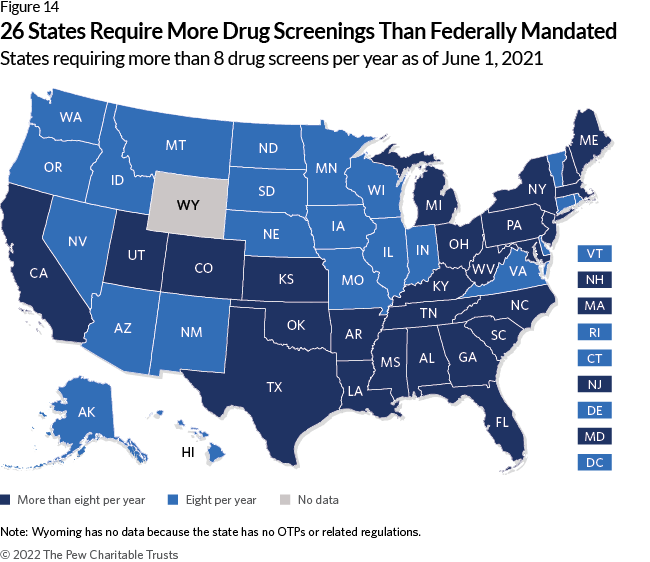
Urine drug screenings
Requiring additional tests
Federal rules require eight drug tests per year.29 Requiring additional tests places a burden on patients and, according to preliminary research, may not be as necessary for patient safety as once thought, and may also raise the cost of treatment.30
Twenty-six states require more than eight annual drug screenings.
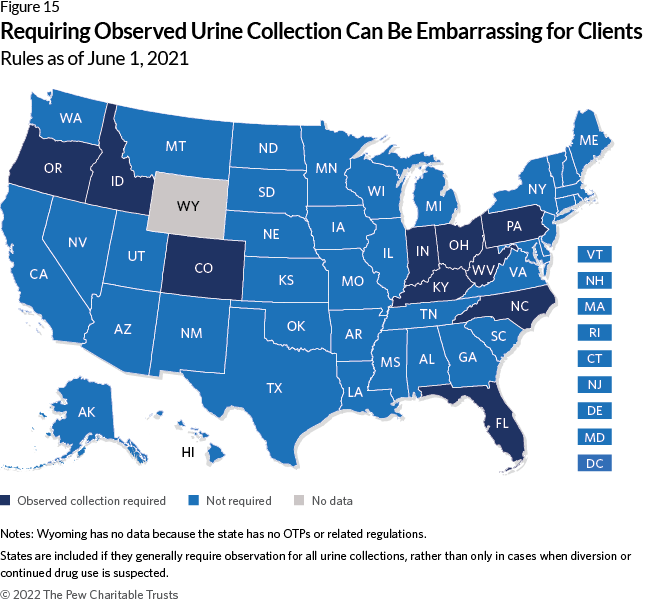
Observing urine specimen collection
Ten states have rules requiring OTPs to observe patients during urine sample collection, which can be embarrassing and degrading for clients.31 According to one, “I don’t like somebody looking at me, or behind me … it’s not a very pleasant experience for anybody. Actually, I think it’s undignified, and I feel it’s wrong.”32
Establishing a treatment goal not based in evidence
Evidence supports that long-term treatment can be more beneficial for patients in terms of overdose risk, employment, health, and criminal justice involvement; according to the American Society of Addiction Medicine, “There is no recommended time limit for pharmacological treatment with methadone.”33
But eight states have rules that establish discontinuation as the goal of treatment. These regulations may encourage providers and patients to stop treatment when doing so is not necessary and can increase overdose death.34
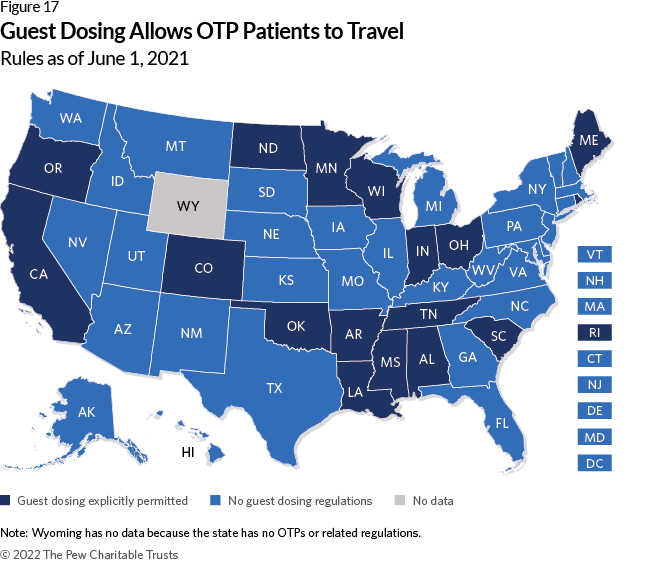
Allowing patients flexibility while traveling
Although other regulations can worsen patient experience, states can also improve it through regulations.
Explicitly allowing guest dosing— that is, temporarily getting methadone from an OTP other than the one at which someone is a patient—is one way to help. This provides flexibility for patients who are traveling.35
Seventeen states have rules that explicitly allow this practice, though it may still be permitted in states without these regulations.
Conclusion
Data shows that many states make it harder for OTP patients to access and remain in treatment in a variety of ways.
As overdose deaths continue to climb, state policymakers should review these rules and make changes so that more people get the lifesaving treatment provided in these settings.
Methodology
Identifying regulatory language
Pew reviewed both statutes and administrative codes for the District of Columbia and all states, except for Wyoming, using Lexis. Wyoming was excluded because the state does not have any OTPs or related regulations.
Initial citations were drawn from Jackson et al. (2020) and the Prescription Drug Abuse Policy System “Requirements for Licensure and Operations of Medications for Opioid Use Disorder Treatment.”36 In addition to these sources, Pew reviewed the section of statutes providing rule-making authority to the agency that promulgated regulations in the administrative code. If either regulations or statutes referred to Board of Pharmacy oversight, Pew also examined the relevant sections of administrative code produced by that body.
Data represents state rules codified in statute and administrative code as of June 2021. It does not reflect any temporary changes such as executive orders or policy statements states may have issued due to the COVID-19 pandemic.37
Coding
Pew developed an initial list of codes based on a review of the OTP federal guidelines and literature on best practices. Using NVivo, the research team that has years of OUD research and policy expertise initially coded five states. The regulations for each state were independently coded by two members of the research team. Pew then held a coding meeting to discuss our findings and refine the codebook, and then recoded these states. The research team then conducted a test of inter-rater reliability, which ensures consistency in coding among research team members, resolved coding discrepancies, and refined the codebook further. Pew then coded five additional states, held another coding meeting, and finalized the codebook. (See Appendix)
Quality control
Pew conducted two quality control steps—comparing our findings with existing research and verifying results with state officials.
Comparison with existing research
Pew compared the findings with previously conducted reviews of OTP regulations.38 In most cases, disagreement between Pew’s findings and these publications were due to differences in definition or because regulations had been updated since those reviews were conducted. If we identified an error based on these comparisons, we updated our data.
Verification with state opioid treatment authorities (SOTAs)
Between June and August 2021, Pew sent the results of each jurisdiction’s regulatory review to their state opioid treatment authority, or SOTA, the official charged with overseeing OTPs. These officials were identified by a list maintained by the Substance Abuse and Mental Health Services Administration.39 For Wyoming, Pew contacted the deputy administrator of the Behavioral Health Division because the state does not have a SOTA.
Each SOTA was asked to verify whether Pew’s interpretation of their state’s OTP rules was correct, and if it was not, to provide updated information.
After sending multiple reminders to each official, Pew received responses from all but 12 states (Delaware, Kansas, Mississippi, Missouri, New Hampshire, New York, Rhode Island, Tennessee, Utah, Vermont, Washington, and Wisconsin). If the SOTA disagreed with the research team’s findings, Pew either updated the research or explained the decision not to. In those cases where we did not update our findings, those discrepancies were either due to differences in definitions or because updated regulatory language was not in effect until after June 1, 2021, our cutoff date.
Endnotes
- The Pew Charitable Trusts, “Medications for Opioid Use Disorder Improve Patient Outcomes” (2020), https://www.pewtrusts.org/en/research-and-analysis/factsheets/2020/12/medications-for-opioid-use-disorder-improve-patient-outcomes.
- The Pew Charitable Trusts, “Improved Opioid Treatment Programs Would Expand Access to Quality Care” (2022), https://www.pewtrusts.org/-/media/assets/2022/03/improve-opioid-treatment-programs-to-expand-access.pdf.
- American Society of Addiction Medicine, “Regulation of the Treatment of Opioid Use Disorder With Methadone” (2021), https://www.asam.org/advocacy/public-policystatements/details/public-policy-statements/2021/11/16/the-regulation-of-the-treatment-of-opioid-use-disorder-with-methadone.
- M. Hawryluk, “Calls to Overhaul Methadone Distribution Intensify, but Clinics Resist,” KHN, March 3, 2022, https://khn.org/news/article/opioid-methadone-treatmentoverhaul-clinics-resist-addiction/.
- J.H. Duff and J.A. Carter, “Location of Medication-Assisted Treatment for Opioid Addiction: In Brief” (Congressional Research Service, 2019), https://www.everycrsreport.com/files/20190624_R45782_ed39091fadf888655ebd69729c3180c3f7e550f6.pdf.
- Substance Abuse and Mental Health Services Administration, “OTP Services Through Medication Units” (2022), https://www.samhsa.gov/medication-assisted-treatment/become-accredited-opioid-treatment-program care; A. McBournie et al., “Methadone Barriers Persist, Despite Decades of Evidence,” Health Affairs Blog, Health Affairs, Sept. 23, 2019, https://www.healthaffairs.org/do/10.1377/hblog20190920.981503/full/#_ftnref1.
- Ohio Administrative Code, Medication Units, 5122-40-15 (2019), https://codes.ohio.gov/ohio-administrative-code/rule-5122-40-15.
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards, https://www.ecfr.gov/cgi-bin/retrieveECFR?gp=3&SID=7282616ac574225f795d5849935efc45&ty=HTML&h=L&n=pt42.1.8&r=PART.
- Ibid.
- University of Florida Health, “What Are the Benefits of Becoming a Consultant Pharmacist?” accessed March 21, 2022, https://cpe.pharmacy.ufl.edu/consultantpharmacist-2/what-are-the-benefits-of-becoming-a-consultant-pharmacist/.
- J.R. Jackson et al., “Characterizing Variability in State-Level Regulations Governing Opioid Treatment Programs,” Journal of Substance Abuse Treatment 115 (2020), https://doi.org/10.1016/j.jsat.2020.108008.
- K. Cioe et al., “A Systematic Review of Patients’ and Providers’ Perspectives of Medications for Treatment of Opioid Use Disorder,” Journal of Substance Abuse Treatment 119 (2020), https://pubmed.ncbi.nlm.nih.gov/33138929; H.S. Reisinger et al., “Premature Discharge From Methadone Treatment: Patient Perspectives,” Journal of Psychoactive Drugs 41, no. 3 (2009): 285-96, https://pubmed.ncbi.nlm.nih.gov/19999682.
- A.M.W. LeBrón et al., “Restrictive ID Policies: Implications for Health Equity,” Journal of Immigrant and Minority Health 20, no. 2 (2018): 255-60, https://doi.org/10.1007/s10903-017-0579-3.
- California Code of Regulations, Patient Identification System, 9 CSR 10240 (2021), https://www.law.cornell.edu/regulations/california/Cal-Code-Regs-Tit-9-SS-10240.
- V. Baaklini et al., “Most States Eased Access to Opioid Use Disorder Treatment During the Pandemic” (2022), https://www.pewtrusts.org/en/research-and-analysis/articles/2022/06/01/most-states-eased-access-to-opioid-use-disorder-treatment-during-the-pandemic.
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards; Substance Abuse and Mental Health Services Administration, “Federal Guidelines for Opioid Treatment Programs” (2015), https://store.samhsa.gov/product/Federal-Guidelines-for-Opioid-Treatment-Programs/PEP15-FEDGUIDEOTP.
- Substance Abuse and Mental Health Services Administration, “Methadone Take-Home Flexibilities Extension Guidance,” last modified March 3, 2022, https://www.samhsa.gov/medication-assisted-treatment/statutes-regulations-guidelines/methadone-guidance.
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards.
- Missouri Code of Regulations, Opioid Treatment Program, 9 CSR 30-3.132 (2021), https://www.law.cornell.edu/regulations/missouri/9-CSR-30-3-132.
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards; M. Hochheimer and G.J. Unick, “Systematic Review and Meta-Analysis of Retention in Treatment Using Medications for Opioid Use Disorder by Medication, Race/Ethnicity, and Gender in the United States,” Addictive Behaviors 124 (2022), https://www.sciencedirect.com/science/article/pii/S0306460321002987.
- Oklahoma Code of Regulations, Service Phases - Phase VI, 450:70-6-17.8 et seq(2021), https://www.law.cornell.edu/regulations/oklahoma/Okla-Admin-CodeSS-450-70-6-17-8 (a sixth phase is also set out in regulations, but new patients have not been eligible for this phase since July 1, 2007).
- National Academies of Sciences, Engineering, and Medicine, Medications for Opioid Use Disorder Save Lives (Washington: National Academies Press, 2019).
- The Pew Charitable Trusts, “Opioid Overdose Crisis Compounded by Polysubstance Use” (2020), https://www.pewtrusts.org/en/research-and-analysis/factsheets/2020/10/opioid-overdose-crisis-compounded-by-polysubstance-use; A.C. Stone et al., “Methadone Maintenance Treatment Among Patients Exposed to Illicit Fentanyl in Rhode Island: Safety, Dose, Retention, and Relapse at 6 Months,” Drug and Alcohol Dependence 192 (2018): 94-97, https://www.sciencedirect.com/science/article/pii/S0376871618304721.
- Substance Abuse and Mental Health Services Administration, “Federal Guidelines for Opioid Treatment Programs”; Substance Abuse and Mental Health Services Administration, “Medications for Opioid Use Disorder: Treatment Improvement Protocol 63” (2021), https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_ Download/PEP21-02-01-002.pdf; National Academies of Sciences, Medications for Opioid Use Disorder Save Lives.
- Substance Abuse and Mental Health Services Administration, “Medications for Opioid Use Disorder: Treatment Improvement Protocol 63.”
- American Society of Addiction Medicine, “National Practice Guideline for the Treatment of Opioid Use Disorder” (2020), https://sitefinitystorage.blob.core.windows.net/sitefinity-production-blobs/docs/default-source/guidelines/npg-jam-supplement.pdf?sfvrsn=a00a52c2_2.
- F. Faggiano et al., “Methadone Maintenance at Different Dosages for Opioid Dependence,” Cochrane Database of Systematic Reviews, no. 3 (2003), https://doi.org//10.1002/14651858.CD002208.
- Substance Abuse and Mental Health Services Administration, “Federal Guidelines for Opioid Treatment Programs”; J.A. Trafton, J. Minkel, and K. Humphreys, “Determining Effective Methadone Doses for Individual Opioid-Dependent Patients,” PLOS Medicine 3, no. 3, (2006): e80, https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0030080.
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards.
- Urban Survivors Union, “The Methadone Manifesto,” (https://sway.office.com/UjvQx4ZNnXAYxhe7?ref=Link&mc_cid=9754583648&mc_eid=51fa67f051; G. Joseph et al., “Reimagining Patient-Centered Care in Opioid Treatment Programs: Lessons From the Bronx During COVID-19,” Journal of Substance Abuse Treatment 122 (2021), https://pubmed.ncbi.nlm.nih.gov/33353790.
- C. Strike and C. Rufo, “Embarrassing, Degrading, or Beneficial: Patient and Staff Perspectives on Urine Drug Testing in Methadone Maintenance Treatment,” Journal of Substance Use 15, no. 5 (2010): 303-12, https://doi.org/10.3109/14659890903431603.
- Ibid.
- National Academies of Sciences, Medications for Opioid Use Disorder Save Lives; American Society of Addiction Medicine, “The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder - 2020 Focused Update” (2020), https://www.asam.org/quality-care/clinical-guidelines/national-practice-guideline.
- N. Krawczyk et al., “Opioid Agonist Treatment Is Highly Protective Against Overdose Death Among a U.S. Statewide Population of Justice-Involved Adults,” The American Journal of Drug and Alcohol Abuse 47, no. 1 (2021): 117-26, https://doi.org/10.1080/00952990.2020.1828440.
- American Association for the Treatment of Opioid Dependence, “AATOD Guidelines for Guest Medication,” http://www.aatod.org/advocacy/policy-statements/aatodguidelines-for-guest-medication/.
- Jackson et al., “Characterizing Variability”; Prescription Drug Abuse Policy System, Requirements for Licensure and Operations of Medications for Opioid Use Disorder Treatment, through Aug. 1, 2020, https://pdaps.org/datasets/medication-assisted-treatment-licensure-and-operations-1580241579.
- American Society of Addiction Medicine, “COVID-19 - National and State Health Guidance,” https://www.asam.org/quality-care/clinical-guidelines/covid/national-andstate-guidance.
- Jackson et al., “Characterizing Variability”; Prescription Drug Abuse Policy System, Requirements for Licensure and Operations of Medications for Opioid Use Disorder Treatment.
- Substance Abuse and Mental Health Services Administration, “State Opioid Treatment Authorities,” https://www.samhsa.gov/medication-assisted-treatment/sota.