Reports Recommend Strong State Policies on Drug Compounding
A look at state regulation and oversight
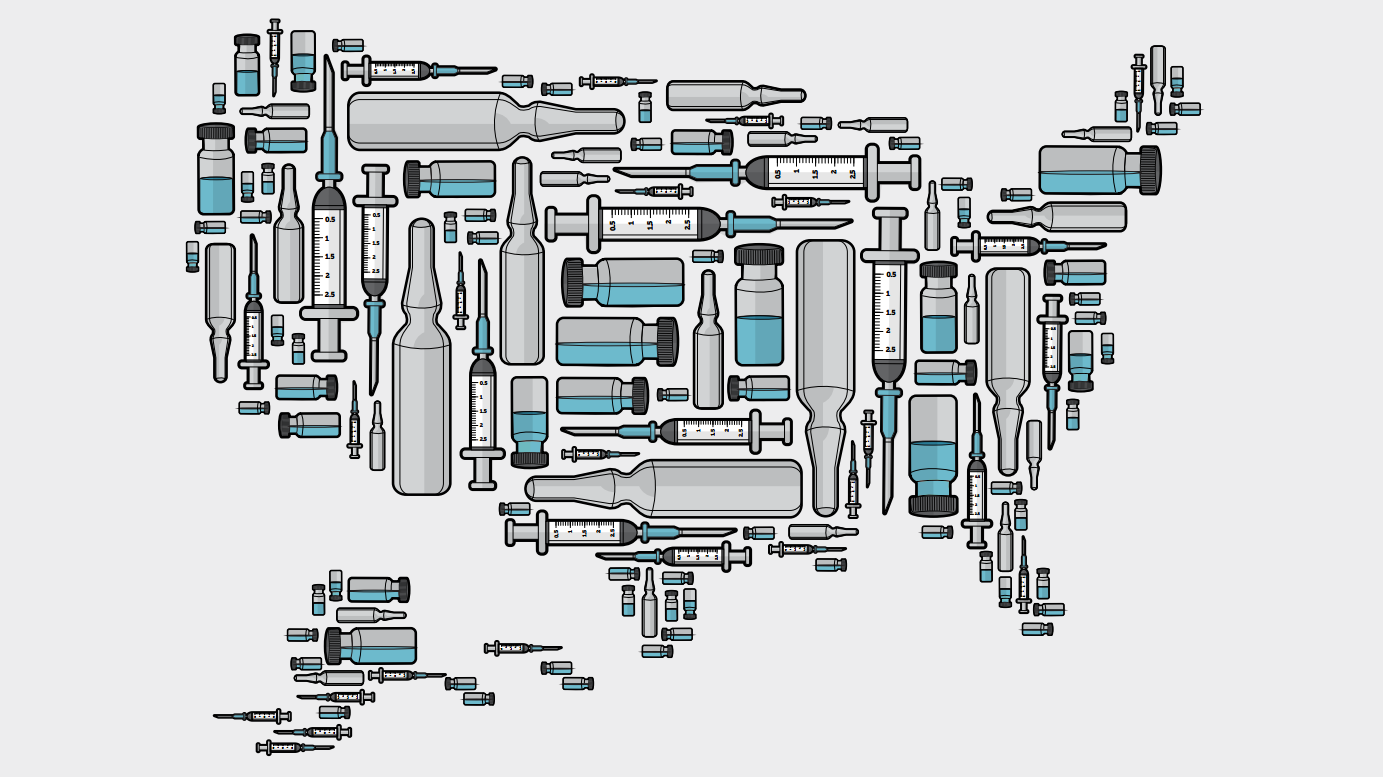
Compounded medications—drugs made by pharmacists, not pharmaceutical manufacturers—grabbed the nation’s attention in 2012, when tainted injections were linked to 64 deaths. In the wake of this incident, Congress and the public demanded proper oversight and better safeguards for compounded medicines.
The Food and Drug Administration (FDA) has the authority to enforce applicable federal laws over pharmacies, but states are the primary regulators of pharmacies, including any small-scale or “traditional” compounding activity. To provide resources for states and other stakeholders, The Pew Charitable Trusts examined states’ oversight policies on compounded drugs, identified their replicable best practices, and detailed these findings in two reports.
The first report, National Assessment of State Oversight of Sterile Drug Compounding, presents research by the University of Illinois at Chicago College of Pharmacy and examines state trends and policy differences. A complementary report, Best Practices for State Oversight of Drug Compounding, looks at the various elements of oversight (e.g., regulations, licensure, and inspection) and offers policy recommendations that were developed by an advisory committee of state pharmacy regulators along with other experts.
National Assessment of State Oversight of Sterile Drug Compounding lays out the differences and similarities among states and the District of Columbia in regulation of compounders and provides a snapshot of the state oversight landscape. Based on data from the 43 participating states, key findings include the following:
- Nearly half of the states have fully adopted the best practice quality standard for compounding sterile drugs (such as injections or infusions), U.S. Pharmacopeial Convention Chapter <797>.
- Just over half of the states inspect in-state pharmacies that perform sterile compounding at least every year, and just over a quarter of states prioritize inspections for high-risk sterile compounding.
- More than half of the states allow traditional pharmacies to compound without a prescription. Such policies may be in conflict with recently clarified federal law.
- Little oversight exists for compounding occurring in doctors’ offices.
Best Practices for State Oversight of Sterile Drug Compounding recommends that states:
- Hold compounding pharmacies to appropriate minimum quality standards and regularly send qualified inspectors to ensure compliance.
- Have systems that track compounding activities in their state, and set meaningful training expectations for pharmacists, especially those who compound sterile drugs.
- Have a mechanism, such as a separate licensure process, to apply and enforce specific standards for facilities that perform sterile compounding.
- Ensure that any policies on compounding without a prescription are aligned with federal law.
- Establish meaningful oversight of any sterile compounding that occurs in doctors’ offices.






