Too Slow
An Analysis of the 2011 Salmonella Ground Turkey Outbreak and Recommendations for Improving Detection and Response
QUICK SUMMARY
Salmonella causes more than 1 million foodborne illnesses every year.1 It is responsible for more hospitalizations and deaths than any other type of bacterium or virus found in food, and its health-related costs to the nation run as much as $11 billion a year.2 Food is estimated to be the source of 90 percent of all salmonella infections, and contaminated poultry is believed to be a main culprit.3,4
A multistate outbreak of Salmonella Heidelberg infections linked to ground turkey in 2011 sickened 136 people, causing 37 hospitalizations and one death. The Pew Charitable Trusts' analysis of the outbreak found numerous inadequacies in the foodborne illness surveillance system that, if addressed, could help to prevent illnesses and, in some cases, deaths.
Executive Summary
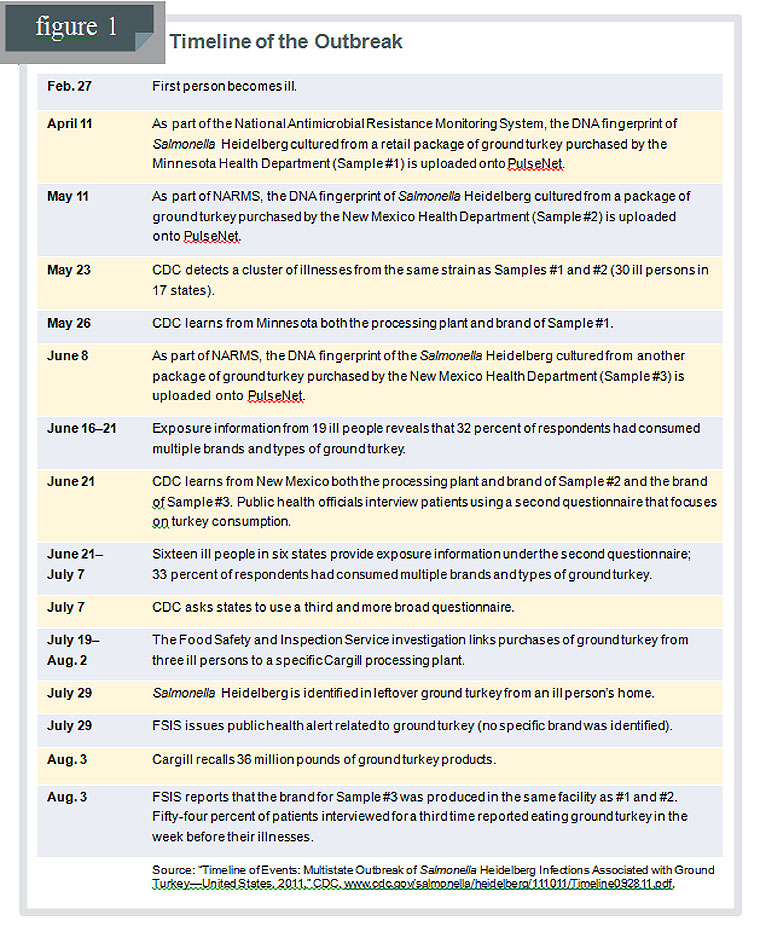
An examination of the timeline for the outbreak reveals that the U.S. Centers for Disease Control and Prevention (CDC) and the U.S. Department of Agriculture's Food Safety and Inspection Service (FSIS) did not identify the contaminated food source—ground turkey processed at one of Cargill Meat Solutions Corp.'s plants — until 22 weeks after the first person became ill and 10 weeks after CDC detected the outbreak. Cargill's subsequent recall of approximately 36 million pounds of ground turkey products is one of the nation's biggest poultry recalls.
The 2011 Salmonella Heidelberg outbreak linked to ground turkey deserves special scrutiny because it highlights several opportunities to improve foodborne illness surveillance, detection, and response.
Pew's examination of this outbreak focuses on three problems in the system as it currently exists:
1. Infections from salmonella are not given enough attention by the public health system and, as a result:
- Public health officials do not always interview patients promptly, missing a critical opportunity to obtain the most accurate information on what they have eaten. In addition, a common set of questions is not used, making it difficult to aggregate and analyze key information.
- Not all states require that samples of salmonella cultured from patients (“isolates”) by clinical laboratories be sent to public health laboratories for further analysis.
- Public health labs do not perform DNA fingerprinting of salmonella isolates received on a universal or timely basis.
2. Bacteria isolated from retail meat and poultry samples and uploaded onto PulseNet — a national network of labs that shares information on foodborne bacteria — are not identified with the names of the brand and processing plants that produced the samples, nor by their purchase dates.i This is the case for other foodborne pathogens, not just salmonella. Delays in the resolution of outbreaks may occur because investigators who rely on PulseNet to find matches of bacteria in humans and other sources do not have ready access to this identifying information. In addition, without these data, there is no ability to detect when a plant repeatedly produces contaminated products.
3. Government officials often wait until they are relatively certain of a likely source of an outbreak before notifying a company that it may have produced the contaminated food. Waiting for certainty in the 2011 ground turkey case resulted in an outbreak lasting months when, with earlier food industry input, it might have been resolved much sooner and thereby prevented many illnesses.
Based on its analysis, Pew makes three general recommendations for improving salmonella outbreak detection and response. These recommendations could inform the CDC's charge under Section 205 of the 2011 FDA Food Safety Modernization Act to evaluate how to "enhance foodborne illness surveillance systems."
1. Federal and state officials should make the detection of and response to salmonella outbreaks a priority by enhancing the surveillance system for these bacteria so that:
- State and local public health officials interview patients as soon as their cases are reported, using a common set of questions to capture data vital to the outbreak investigation.
- All states require clinical labs to submit their salmonella isolates to public health laboratories.
- Public health labs quickly conduct DNA fingerprinting for all salmonella isolates they receive.
2. The U.S. Food and Drug Administration (FDA) should modify the retail arm of the National Antimicrobial
Resistance Monitoring System (NARMS) so that it can be used to help detect and respond to outbreaks. Specifically, FDA should require that information on the brand, processing plant, and purchase date for meat and poultry retail samples be included when the DNA fingerprint of bacteria isolates are uploaded to PulseNet. Moreover, the DNA fingerprints should be uploaded more quickly.
3. FDA, FSIS, CDC, and state authorities must develop a mechanism that facilitates engagement with food companies in the early stages of an outbreak investigation when information, such as production schedules and distribution patterns, could speed identification of contaminated foods.
Pew's recommendations for surveillance improvements target key points in this outbreak investigation in which existing policies and practices resulted in unnecessary delays and preventable illnesses. While resource constraints could make these recommendations difficult for some states to achieve, in light of the staggering health-related costs of foodborne illnesses, stopping outbreaks as soon as possible will save money and protect the public.
i - The samples are originally collected under the retail arm of the National Antimicrobial Resistance Monitoring System, a national public health surveillance system that tracks antibiotic resistance in foodborne bacteria. The NARMS program was established in 1996 as a partnership between the U.S. Food and Drug Administration, the Centers for Disease Control and Prevention, and the U.S. Department of Agriculture. NARMS monitors antimicrobial susceptibility among enteric bacteria from humans, retail meats, and food animals.
FULL REPORT
Background
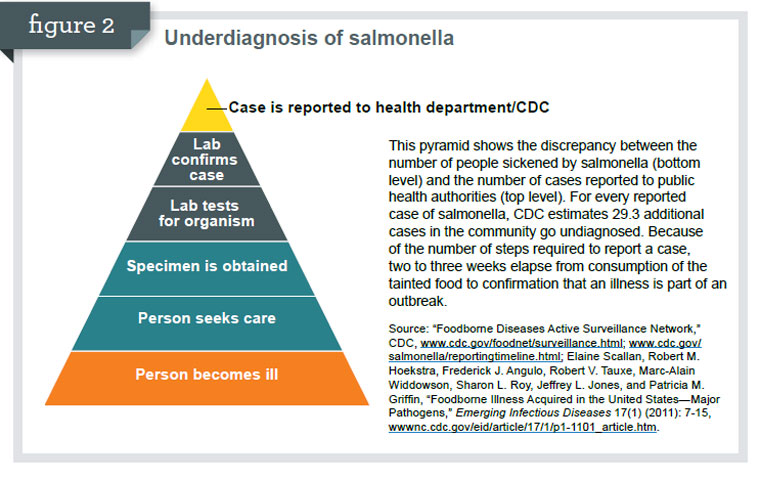
In 2011, a multistate foodborne illness outbreakii of infections caused by Salmonella Heidelberg bacteria sickened 136 persons in 34 states. Thirty-seven people were hospitalized, and one person died. However, these numbers represent only those illnesses actually reported to public health authorities. Based on CDC estimates, due to the underdiagnosis of salmonella5 (see Figure 2), this outbreak could have sickened 4,000 people nationally. In addition, the outbreak's strain of Salmonella Heidelberg was resistant to several commonly prescribed antibiotics.6
About Our Report
Pew staff reviewed and analyzed a series of public documents regarding the 2011 Salmonella Heidelberg outbreak and the health community's response to it, including detailed timelines produced by CDC. Reports and data collected by the Association of Public Health Laboratories (APHL) and peer-reviewed literature that describes the current system for foodborne disease surveillance in the United States were also evaluated. Pew based its observations, conclusions, and recommendations on its staff's professional expertise, as well as on detailed correspondence, conversations, and input from many stakeholders involved in public health, the food industry, and its regulation.
Craig Hedberg, Ph.D., Division of Environmental Health Sciences, University of Minnesota School of Public Health, and Ian Williams, Ph.D., chief of the Outbreak Response and Prevention Branch of the National Center for Emerging and Zoonotic Infectious Diseases at CDC, peer-reviewed the report. Hedberg served on Cargill's expert review panel assembled post-outbreak to review the company's entire process from live-animal operations through ground turkey production. Williams heads the CDC team that investigates all multi-state outbreaks of foodborne illness. Additional reviewers included staff with the U.S. Food and Drug Administration, U.S. Department of Agriculture's Food Safety and Inspection Service, CDC, APHL, and Cargill Meat Solutions Corp.
Multistate outbreaks of foodborne illness such as this are only about 1 percent7 of those reported to CDC each year.iii However, because they involve illnesses nationwide and over a single time period, these events tend to attract the attention of consumers, the news media, and policymakers. According to CDC, these outbreaks have been identified more easily in recent years due to improved surveillance of foodborne disease resulting in detection of a cluster of illnesses that previously would have been missed. Additionally, these outbreaks could be occurring more often because of our increasingly centralized food supply, which results in contaminated products being shipped to many states, making people ill across the country.8
A goal in any outbreak investigation is to quickly identify the contaminated food and remove it from the market; the faster this is done, the fewer people will get sick, because contaminated food will remain in stores and pantries until a recall is widely publicized. The timeline for the Salmonella Heidelberg outbreak reveals that, while the first person became ill Feb. 27, 2011, the contaminated food source — ground turkey processed at Cargill Meat Solutions' plant P-963 in Springdale, AR — was not identified until 22 weeks later. On Aug. 3, Cargill undertook one of the biggest poultry recalls—approximately 36 million pounds of ground turkey products. (See Figure 1 for a detailed timeline of the outbreak.)
ii - An outbreak occurs when two or more people get the same illness from the same contaminated food or drink.
iii - The vast majority of outbreaks are restricted to a county or a state and traditionally do not substantially involve CDC, which focuses only on multistate incidents.
Recommendations and Discussion
The Salmonella Heidelberg outbreak linked to ground turkey is only one of the numerous foodborne multistate outbreaks reported by CDC in 2011,9 but it deserves special scrutiny because it highlights several opportunities for improving foodborne illness surveillance, detection, and response, especially as they relate to salmonella outbreaks.
| Some of the high-profile multistate foodborne outbreaks of 2011 as reported by CDC | |
| • Ground beef — Salmonella Typhimurium • Romaine lettuce — Escherichia coli O157:H7 • Kosher broiled chicken livers — Salmonella Heidelberg • Turkish pine nuts — Salmonella Enteritidis • Jensen Farms cantaloupes — Listeria monocytogenes • Ground turkey — Salmonella Heidelberg • Whole, fresh imported papayas — Salmonella Agona • Alfalfa and spicy sprouts — Salmonella Enteritidis • Turkey burgers — Salmonella Hadar • Lebanon bologna — E. coli O157:H7 • Del Monte cantaloupe — Salmonella Panama • Hazelnuts — E. coli O157:H7 Source: “Multistate Foodborne Outbreak Investigations,” CDC, accessed June 14, 2012,http://www.cdc.gov/foodsafety/outbreaks/multistate-outbreaks/outbreaks-list.html |
|
Before an analysis of the detection of and response to this outbreak, it is important to underscore that this report focuses primarily on what happens once people become ill from contaminated food; it does not address how to prevent that contamination. An examination of the latter issue should include an assessment of the effectiveness of existing government food safety regulations and policies. USDA's Food Safety and Inspection Service — the agency responsible for overseeing the safety of meat and poultry products — has adopted an array of food safety regulations, including performance standards that limit the prevalence of particular pathogens in meat and poultry products. These standards serve as the measures for determining whether a company is producing safe food.10 Currently, the performance standard for salmonella in raw ground turkey is 49.9 percent11 — meaning that it is lawful for nearly half of the samples tested by the Food Safety and Inspection Service to be contaminated with salmonella. This standard is based on data collected 17 years ago that estimated the national prevalence of salmonella in raw ground turkey at the time.12
The 2011 Cargill ground turkey outbreak clearly calls into question the effectiveness of this standard in protecting public health and illustrates the need to have policies that are directly related to public health and to regularly update them to reflect industry advances, thereby encouraging constant improvement.iv
Congress has recently required CDC to evaluate how it can improve the current system that it uses to detect illnesses caused by contaminated food. Section 205 of the FDA Food Safety Modernization Act, enacted in January 2011, directs CDC to work with federal and state food safety agencies to "enhance foodborne illness surveillance systems to improve the collection, analysis, reporting, and usefulness of data on foodborne illnesses."13
Based upon this analysis of the events surrounding the outbreak, Pew recommends that, consistent with congressional intent, CDC as well as the states consider implementing the following strategies aimed at improving detection of and response to salmonella outbreaks.
Recommendation 1
Federal and state officials should make the detection of and response to salmonella outbreaks a priority by enhancing the surveillance system for these bacteria so that:
- State and local public health officials interview patients as soon as their cases are reported using a common set of questions in order to capture data vital to the outbreak investigation.
- All states require clinical labs to submit their salmonella isolates to public health laboratories.
- Public health labs quickly conduct DNA fingerprinting for all salmonella isolates they receive.
Salmonella results in more hospitalizations and deaths than any other type of bacterium or virus found in food, which is the source for 90 percent of all salmonella infections. According to CDC, salmonella annually causes 1.23 million illnesses, 23,128 hospitalizations, and 452 deaths in the United States.14Outbreaks of salmonella have been associated with a number of food products, from jalapeño peppers to salami.15 However, poultry is considered a main source of the contamination — responsible for more than one-fifth of illnessesv — in the United States.16 In addition, according to a risk-ranking study conducted by the University of Florida, salmonella in poultry ranked fourth among 168 pathogen-food combinations analyzed.17
Significant progress has been made over the past 15 years in lowering the incidence of foodborne infections from Escherichia coli O157:H7, which causes one of the most serious foodborne illnesses. The rate of infections in 2010 has decreased by 44 percent compared with 1996-98 rates.18 In 2010, the incidence of E. coli O157:H7 was 0.9 cases per 100,000, which met the Healthy People 2010vi target of 1.0.19 For 2020, the new target for E. coli O157:H7 is 0.6 cases per 100,000.20 The successful reduction in the rate of infections was achieved through a combination of enhanced government and industry oversight of the slaughter process as well as USDA's decision to declare this pathogen an adulterant when it is found in beef trimmings and ground meat. Changes in processing practices for cattle, the main source of this pathogen, also played a role.
By contrast, the incidence of foodborne infections from salmonella has not decreased significantly. In 2010, the incidence was 17.6 cases per 100,000,21 more than twice the Healthy People 2010 objective of 6.8 cases per 100,000.22 The new national health target for 2020 aims for 11.4 cases of salmonella infection per 100,000, only a 25 percent reduction in the incidence reported from 2006 to 2008.23 As these statistics demonstrate, there has not been significant progress in lowering the rate of salmonella infections. Efforts to reduce this pathogen face particular challenges because so many animals can carry it and it can be present in organs other than the intestines, complicating control strategies.
| More on Salmonella | |
| The salmonella genus includes more than 2,300 variations, or serotypes, of bacteria. Strains that cause no symptoms in animals can make people sick, and vice versa. If present in food, salmonella does not usually affect the taste, smell, or appearance of food. The bacteria live in the intestinal tracts of infected animals and humans. Two serotypes of salmonella account for half of all human infections. Source: “Salmonella Questions and Answers,” Food Safety and Inspection Service, accessed June 12, 2012, www.fsis.usda.gov/factsheets/salmonella_questions_&_answers. |
|
At the state and local level, a series of delays and inconsistencies in the surveillance system impeded epidemiologists from quickly detecting and responding to the 2011 ground turkey outbreak. In general, state public health laboratories do not give salmonella outbreaks the urgent attention that E. coli O157:H7 and Listeria cases receive.24 Budget cuts at the state level have resulted in some public health labs reducing their activities related to PulseNet,25 a national network of public health and food regulatory agency laboratories coordinated by CDC. State health departments electronically submit the DNA fingerprints of foodborne disease-causing bacteria that have been cultured from patients and other sources by uploading them on PulseNet. These fingerprints distinguish strains or organisms at the DNA level, and CDC uses this information to determine whether an outbreak is occurring. Through PulseNet, CDC detects about 70 percent of the multistate outbreaks.26
Unpublished data from the Association of Public Health Laboratories reveal that 30 percent of state labs do not perform DNA fingerprinting on all of the salmonella isolates they receive.27 As a result, an outbreak requires more cases in these states before it is detected. Furthermore, while the average wait for the DNA fingerprint of a salmonella isolate to be completed and uploaded on PulseNet is five days, the process might take as long as 19 working days, depending on the state. Not all states even require clinical labs to submit their isolates to a public health laboratory; Twelve states and the District of Columbia do not require salmonella isolates to be submitted. The fact that not all foodborne pathogen isolates undergo further molecular analysis delays the detection of outbreaks, probably allowing some to go undetected. Furthermore, although every state reports cases of salmonella to CDC, the allowable period in which health care providers must report varies widely, with 45 percent of the states requiring a report within 24 hours. Fifteen other states (30 percent) allow up to a week for salmonella cases to be reported.28
| Although every state reports cases of salmonella to CDC, the allowable period in which health care providers must report varies widely, with 45 percent of the states requiring a report within 24 hours. Fifteen other states (30 percent) allow up to a week for salmonella cases to be reported. |
Whether an outbreak affects a single state or is multistate in scope, state and local investigators interview patients to collect the information that helps resolve the outbreak. The speed of the CDC investigation depends on how quickly state and local officials talk to patients and submit the information to CDC. In an era of inadequate resources, state and local health departments are not always able to provide a quick turnaround. Exacerbating matters, states do not ask victims the same set of questions to help identify the source of the outbreak. As a result, CDC must take extra time to aggregate and analyze the information.
In 2005, CDC launched its Listeria Initiative,vii an enhanced surveillance system that collects reports of laboratory-confirmed cases caused by the pathogen. As part of this initiative, state and local health departments are encouraged to follow up on all Listeria patients as soon as their cases are reported, and to collect relevant data using an extended questionnaire.29,30 This enhanced surveillance system made a substantial contribution to the relatively quick resolution of aListeria outbreak linked to cantaloupes in the summer of 2011.31
The 2011 Cargill ground turkey outbreak highlights the need to make a significant reduction of salmonella infections a public health priority.32,33 Toward this end, CDC should enhance the surveillance system for salmonella following the model of that used for Listeria, which would include directing state and local officials to redouble their surveillance efforts to detect and respond to foodborne salmonella infections.
Enhancing salmonella surveillance would require significant investment; however, adequate resources and sufficient attention focused on this pathogen — which costs the nation as much as $11 billion a year34 — would lead to significant improvements in public health. What would be learned through this robust effort would improve the response to outbreaks and generate better data with which to develop a prevention-based food safety system.
Recommendation 2
The U.S. Food and Drug Administration should modify the retail arm of the National Antimicrobial Resistance Monitoring System so that it can help detect and respond to outbreaks. Specifically, FDA should require that information on the brand, processing plant, and purchase date of meat and poultry retail samples be included when the DNA fingerprint of bacteria isolates are uploaded to PulseNet. Moreover, the DNA fingerprints should be uploaded more quickly.
When CDC first detected the contaminated ground turkey cluster on May 23, 2011, Salmonella Heidelberg isolates from two ground turkey products exactly matched those obtained from patients. These samples, obtained through the arm of NARMS that monitors retail meats, had been uploaded onto PulseNet on April 11 and May 11, about a month after each retail sample had been collected. Although the brand and processing plant are routinely captured as part of the sample identification, this information is not uploaded with the isolate. As a result, CDC did not become aware of this critical information until May 26 and June 21, respectively, and only after it requested the details.viii
NARMS monitors trends in antimicrobial resistance among foodborne bacteria. Three federal agencies share responsibility for the monitoring system: CDC is responsible for samples collected from humans, USDA does so for animals, and FDA for retail meats.ix Because NARMS was not established to identify specific contamination events in real time, it can take a month or more — as was the case in this outbreak — for DNA fingerprints from microorganisms cultured from retail meat samples to be added to PulseNet. Currently, CDC must ask the state that collected the retail sample for information on brand name and processing plant, potentially further delaying a resolution to the investigation. Access to purchase dates is also important because they can verify that a product was bought before the onset
of illness. Without this information, it is not possible to track instances in which a plant repeatedly manufactures contaminated product.
Matches between NARMS' retail meat samples and outbreak strains are commonly found during investigations. Although these matches alone do not provide sufficient evidence to solve an outbreak, they can help generate a hypothesis for the cause of the outbreak. Epidemiologists use more than just NARMS' data as the basis for determining a likely food source of an outbreak. There must also be data relating the illnesses to the contaminated food, records that trace the product back to the source, and microbiological test results from the suspected food item that match the outbreak strain.
While NARMS was not designed to be an outbreak surveillance program, its retail arm could be modified to serve as a more helpful tool. Posting DNA fingerprints along with brand name, processing plant, and purchase date information on PulseNet in a timely fashion would make this information readily available during outbreak investigations.
Recommendation 3
FDA, FSIS, CDC, and state authorities must develop a mechanism that facilitates engagement with food companies in the early stages of an outbreak investigation when information such as production schedules and distribution patterns could speed identification of contaminated foods.
During the ground turkey outbreak, retail samples from Cargill establishment P-963 collected by the retail arm of NARMS repeatedly tested positive for the outbreak strain. The company, however, did not learn of this or any other aspects of the outbreak investigation until shortly before it initiated the recall on Aug. 3.
During many outbreaks, FDA or FSIS contacts a food company, but only after the agencies and CDC have identified a likely source of the outbreak that implicates that company. A more effective strategy would be for regulatory agencies, CDC, and state officials to contact food industry representatives much earlier. In this case, if industry had been contacted in mid-June when three NARMS retail samples were found to match the illness strain and patients reported higher-than-expected ground turkey consumption,x turkey processors could have helped investigators narrow the potential food sources by sharing relevant production and distribution data. For example, the companies might have provided helpful microbiological testing data for turkeys (before and after slaughter) and ground turkey products.
A mechanism should be created to facilitate the sharing of relevant data in real time on a regular basis among regulatory agencies, CDC, and the food industry. In Britain, government agencies and industry convene "scoping groups" at the beginning of an outbreak to share information and narrow the possible food items that could be involved.
Food companies' best interests would be served by consulting with CDC early in an outbreak investigation, because quicker resolution and targeted messages to consumers could limit companies' losses. For example, in the first weeks of the 2008 Salmonella Saintpaul outbreak, in which tomatoes were a suspected source, produce industry repesentatives made available to FDA a list of the states, territories, and countries producing tomatoes not implicated in the outbreak, which the agency then published to direct consumers to safe products. Tomato growers also provided information related to production, processing, and distribution.35
A number of issues need to be addressed before an early consultation mechanism could be adopted in the United States. The roles to be played in this process by regulatory and enforcement agencies need to be defined. The level of evidence required to identify a food item as a likely source of an outbreak should be clearly delineated. In addition, industry's concerns about whether sharing information could expose it to enforcement actions must be addressed. At the same time, lessons from other outbreaks make two things clear: Industry should not be allowed to demand that the exchange of data be contingent on CDC's agreement to withhold the names and locations of implicated companies, and industry should not in any way pressure CDC to delay actions or public announcements related to an outbreak. The proper role of consumers and public health organizations in this consultative process must also be determined.
iv - The Food Safety and Inspection Service announced on Dec. 6, 2012, that it will begin sampling to determine the prevalence of salmonella in “comminuted” (raw ground and similar non-intact product) poultry and will use the data collected to develop new performance standards. It is likely to also develop standards for the bacteria campylobacter. For more on the announcement, go to www.fsis.usda.gov/OPPDE/rdad/FRPubs/2012-0007.pdf.
v - This estimate is based on data from foodborne disease outbreaks reported to CDC.
vi- "Healthy People" reports provide science-based, 10-year national objectives for improving the health of all Americans. An effort of the U.S. Department of Health and Human Services, Healthy People establishes benchmarks and monitors progress. More on the Healthy People targets atwww.healthypeople.gov/2020/default.aspx.
vii - The Listeria Initiative was piloted in the Foodborne Diseases Active Surveillance Network (FoodNet) in 2004 and implemented nationwide in 2005. The number of states participating in and the number of reports sent to the Listeria Initiative continue to increase. More information can be found atwww.cdc.gov//listeria//pdf//ListeriaInitiativeOverview_508.pdf.
viii - A third retail sample was uploaded onto PulseNet on June 8 that also matched the outbreak strain. The processing plant for this particular sample was not identified as P-963—the same plant as the two previous retail samples—until Aug. 3. During the outbreak, five ground turkey samples were purchased from five retail locations but all from the same processing plant that yielded the outbreak strain.
ix - CDC conducts the antimicrobial tests on human samples. For animal isolates, USDA's Agricultural Research Service does the testing, and the National Veterinary Services Laboratories does the serotyping. Participating FoodNet sites and other state public health departments purchase and culture the retail meat samples and then send the isolates to FDA for testing. More information can be found atwww.fda.gov/AnimalVeterinary/SafetyHealth/AntimicrobialResistance/
NationalAntimicrobialResistanceMonitoringSystem/ucm059089.htm.
x - The first round of patient interviews conducted by state investigators revealed that 32 percent reported eating ground turkey, a consumption rate significantly higher than the 11 percent estimated by CDC for ground turkey on the Population Survey Atlas of Exposures, 2006-2007, which can be found atwww.cdc.gov/foodnet/PDFs/FNExpAtl03022011.pdf.
The 2011 Salmonella Heidelberg outbreak linked to ground turkey illustrates several shortcomings in the nation's surveillance efforts of foodborne illnesses. These gaps lead to unnecessary investigative delays and carry a cost in human illness and loss of life. The recommendations made here are varied: Some are relatively straightforward and probably will not demand significant resources, while others will require investments to meaningfully reduce the burden of salmonella in the United States. Nevertheless, the expense to society attributable to salmonella infections — estimated at as much as $11 billion a year in health-related costs alone36 — clearly justifies dedicating more funding to the prevention of these illnesses.
April 2013
The Pew Charitable Trusts is driven by the power of knowledge to solve today's most challenging problems. Pew applies a rigorous, analytical approach to improve public policy, inform the public, and stimulate civic life.
The food safety project seeks to reduce health risks from foodborne pathogens by strengthening federal government authority and the enforcement of food safety laws.
The Pew Charitable Trusts
Susan K. Urahn, executive vice president
Erik Olson, deputy director of food programs
The food safety project — Sandra Eskin, Juliana Ruzante, Colin Finan, and Ben Kessler — would like to thank Pew staff members Pete Janhunen, Juli Putnam, Joshua Wenderoff, Lisa Gonzales, and Liz Visser for providing valuable feedback on the report, and Natalia Pelayo and Steve Howard for Web support. Our thanks also go to designer Penelope Malish and fact checker Betsy Towner Levine.
The report benefited from the insights and expertise of external reviewers Craig Hedberg, Ph.D., professor in the School of Public Health at the University of Minnesota, and Ian Williams, Ph.D., chief of the Outbreak Response and Prevention Branch, National Center for Emerging and Zoonotic Infectious Diseases at the U.S. Centers for Disease Control and Prevention.
For additional information, please visit pewhealth.org/foodsafety.
REFERENCES
1. Elaine Scallan, Robert M. Hoekstra, Frederick J. Angulo, Robert V. Tauxe, Marc-Alain Widdowson, Sharon L. Roy, Jeffery L. Jones, and Patricia M. Griffin, “Foodborne Illness Acquired in the United States — Major Pathogens,” Emerging Infectious Diseases 17 (2011): 7-15.
2. Robert L. Scharff, “Economic Burden from Health Losses Due to Foodborne Illness in the United States,” Journal of Food Protection 75 (2012): 123-131.
3. Shua J. Chai, Patricia L. White, Sarah L. Lathrop, Suzanne M. Solghan, Carlota Medus, Beth M. McGlinchey, Melissa Tobin-D'Angelo, Ruthanne Marcus, and Barbara E. Mahon, “Salmonella enterica Serotype Enteritidis: Increasing Incidence of Domestically Acquired Infections,” Clinical Infectious Diseases 54 (2012): S497.
4. Michael B. Batz, Sandra Hoffmann, and J. Glenn Morris, Jr., “Ranking the Risks: The 10 Pathogen-Food Combinations With the Greatest Burden on Public Health,” 2011, accessed June 14, 2012, www.folio.iupui.edu/bitstream/handle/10244/1022/72267report.pdf.
5. Scallan et al., “Foodborne Illness Acquired in the United States—Major Pathogens,” 7-15.
6. “Investigation Update: Multistate Outbreak of Human Salmonella Heidelberg Infections Linked to Ground Turkey,” Centers for Disease Control and Prevention, accessed June 14, 2012, www.cdc.gov/Salmonella/heidelberg/111011.
7. Rendi Murphree, Katie Garman, Quyen Phan, Karen Everstine, L. Hannah Gould, and Timothy F. Jones, “Characteristics of Foodborne Disease Outbreak Investigations Conducted by Foodborne Diseases Active Surveillance Network (FoodNet) Sites, 2003-2008,”Clinical Infectious Diseases 54 (2012): S503.
8. “Multistate Foodborne Outbreaks: CDC's Role,” Centers for Disease Control and Prevention, accessed Nov. 9, 2012, http://www.cdc.gov/foodsafety/outbreaks/multistate-outbreaks/cdc-role.html.
9. “Multistate Foodborne Outbreak Investigations,” Centers for Disease Control and Prevention, accessed June 14, 2012, www.cdc.gov/outbreaknet/outbreaks.html.
10. Pathogen Reduction; Hazard Analysis and Critical Control Point (HACCP) Systems; Final rule No. 144, 9 C.F.R. 304 (July 25, 1996).
11. Contamination with Microorganisms; Process Control Verification Criteria and Testing; Pathogen Reduction Standards; 9 C.F.R. 381.94.
12. Food Safety and Inspection Service, “Nationwide Raw Ground Turkey Microbiological Survey,” 1996, accessed Oct.
11, 2012, www.fsis.usda.gov/OPHS/baseline/rwgrturk.pdf.
13. Section 205 of the FDA Food Safety Modernization Act; Public Law 111-353, 124 STAT. 3885 (Jan. 4, 2011).
14. Scallan et al., “Foodborne Illness Acquired in the United States—Major Pathogens,” 7-15.
15. “Reports of Selected Salmonella Outbreak Investigations,” Centers for Disease Control and Prevention, accessed June
14, 2012, www.cdc.gov/salmonella/outbreaks.html.
16. Batz et al., “Ranking the Risks: The 10 Pathogen-Food Combinations With the Greatest Burden on Public Health,”
2011.
17. Batz et al., “Ranking the Risks: The 10 Pathogen-Food Combinations With the Greatest Burden on Public Health,”
2011.
18. Centers for Disease Control and Prevention, “Vital Signs: Incidence and Trends of Infection With Pathogens Transmitted Commonly Through Food — Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 1996-2010,” Morbidity and Mortality Weekly Report 60 (2011): 749-755, accessed Dec. 12, 2012, http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6022a5.htm.
19. Centers for Diseases Control and Prevention, “Healthy People 2010: Final Review,” 2010, accessed June 16, 2012, www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf.
20. “Healthy People 2020 Topics & Objectives,” Centers for Disease Control and Prevention, accessed June 18, 2012, http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=14.
21. Centers for Disease Control and Prevention, “Vital Signs: Incidence and Trends of Infection With Pathogens Transmitted Commonly Through Food—Foodborne Disease Active Surveillance Network, 10 U.S. Sites, 1996-2010,” 749-755.
22. “Healthy People 2010: Final Review.”
23. “Healthy People 2020 Topics & Objectives.”
24. Council of State and Territorial Epidemiologists, “2010 Food Safety Epidemiology Capacity Assessment,” 2010, accessed June 12, 2012, http://www.cste2.org/webpdfs/fseca.pdf.
25. David Boxrud, Timothy Monson, Tracy Stiles, and John Besser, “The Role, Challenges, and Support of PulseNet Laboratories in Detecting Foodborne Disease Outbreaks,” Public Health Reports 125 (2010): 57-62.
26. Ian Williams, e-mail message, Feb. 15, 2012.
27. This data comes from a survey done by the Association of Public Health Laboratories. Out of 55 PulseNet laboratories,
41 agreed to provide their survey information to Pew.
28. Max Levy, Joe Yerardi, and Dustin Volz, “Flawed State Reporting Leaves Consumers Vulnerable,” News21, accessed June 12, 2012, http://foodsafety.news21.com/2011/response/analysis.
29. A video on how contaminated food is identified during an outbreak can be found at http://www.youtube.com/watch?v=XKD7eNn8bFs.
30. “Multistate and Nationwide Foodborne Outbreak Investigations: A Step-by-Step Guide.” Centers for Disease Control and Prevention, accessed March 8, 2013, http://www.cdc.gov/foodsafety/outbreaks/investigating-outbreaks/investigations/index.html.
31. “Multistate Outbreak of Listeriosis Linked to Whole Cantaloupes From Jensen Farms, Colorado,” Centers for Disease Control and Prevention, accessed June 14, 2012, http://www.cdc.gov/listeria/outbreaks/cantaloupes-jensen-farms/index.html?s_cid=cs_654.
32. Chai et al., “Salmonella enterica Serotype Enteritidis: Increasing Incidence of Domestically Acquired Infections,” S497.
33. “Making Food Safer to Eat: Reducing Contamination from the Farm to the Table,” Centers for Disease Control and Prevention, accessed June 14, 2012, http://www.cdc.gov/vitalsigns/foodsafety/.
34. Scharff, “Economic Burden from Health Losses Due to Foodborne Illness in the United States,” 123-131.
35. “FDA Warns Consumers Nationwide Not to Eat Certain Types of Raw Red Tomatoes,” U.S. Food and Drug Administration, accessed June 18, 2012, http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116908.htm.
36. Scharff, “Economic Burden from Health Losses Due to Foodborne Illness in the United States,” 123-131.









