The Threat of Multidrug-Resistant Infections to the U.S. Military
Expert Testimony, Research, and Commentary
“MDRO [multidrug-resistant organism] infections have become an international health problem during the past several decades and now pose a challenge to the care of our wounded military personnel.”
— D. Hospenthal et al., “Multidrug-resistant Bacterial Colonization of Combat-Injured Personnel at Admission to Medical Centers After Evacuation from Afghanistan and Iraq,” Journal of Trauma, July 2011
“The increase in MDRO infections has resulted in a shortage of safe and effective antibiotics. . . . While both civilian and DOD [Department of Defense] hospitals are dealing with this challenging epidemic, the demographics of patients with MDRO infections are different. Most U.S. hospitals have reported these problems among patients with an increased length of stay, frequently the elderly, with multiple complicated medical problems and usually in an intensive care unit. Military hospitals experience cases of MDRO infections occurring in the younger, combat-injured patients. MDROs complicate chronic skin and soft tissue infections, osteomyelitis, and, in some of the injured, led to increased limb loss, sepsis, and death.”
— Witness Statement of Colonel (Dr.) James Collier and Lieutenant Colonel (Dr.) Michael Forgione, United States Air Force, before the House Armed Services Subcommittee on Oversight and Investigations, September 29, 2010
“Since the onset of Operations Iraqi Freedom and Enduring Freedom, infection and colonization with MDROs . . . have complicated the care of injured U.S. military personnel returning from Iraq and Afghanistan.”
— Witness Statement of Colonel Duane R. Hospenthal, M.D., Ph.D., United States Army, Infectious Disease Consultant to the Army Surgeon General and Chief, Infectious Disease, Brooke Army Medical Center, Fort Sam Houston, Texas, and Colonel Jonathan Jaffin, M.D., United States Army, Director, Health Policy and Services, Office of the Army Surgeon General, before the House Armed Services Subcommittee on Oversight and Investigations, September 29, 2010
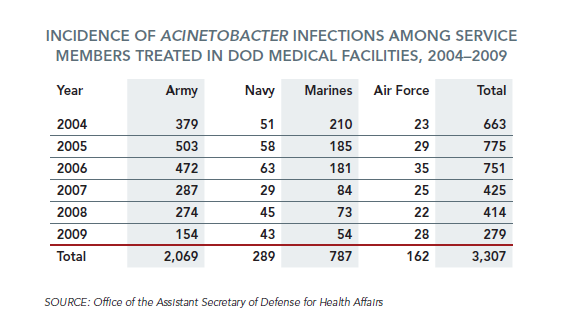
“According to available data from the Department of Defense, approximately 3,300 service members that were treated in military treatment facilities during 2004-2009 had Acinetobacter infections.”
— Memorandum on DOD's Response to Multidrug-resistant Infections in Military Hospitals, Subcommittee on Oversight and Investigations, House Committee on
Armed Services, U.S. House of Representatives, December 6, 2010
“Since the U.S. military entered Afghanistan and Iraq, the military health systems in these countries have experienced a marked increase in nosocomial wound and health-care-associated infections caused by Gram-negative multidrug-resistant (MDR) organisms with very limited treatment options. . . . These MDR organisms often invoke a panoply of mechanisms against the same antibiotic, or use a single mechanism to neutralise several antibiotics, especially in the presence of antibiotic
selection pressure. The dry pipeline of research and development for new antibiotic compounds further exacerbates this crisis.”
— E. Lesho et al., “Surveillance, characterisation, and preservation of multidrug-resistant bacteria,” The Lancet Infectious Diseases, Volume 11, January 2011
“In 2010, treating infections in the setting of widespread bacterial resistance has challenged the Military Health System (MHS) as it has hospitals throughout the U.S. and rest of the world. The difference for the Department of Defense (DOD) has been the concomitant care of thousands of young, injured service members coming from the wars in Iraq and Afghanistan. Increasingly, many of these critically injured patients are colonized or infected with MDROs, especially gram-negative bacteria, that demonstrate resistance not just to first-line antibiotics, but to all the major antibiotic classes in our armamentarium. This situation limits treatment options with either second-line drugs with greater toxicity or, in some cases, no drugs to which the organism demonstrates sensitivity. . . . Persistent infections, prolonged hospitalizations, more numerous and extensive surgical procedures, and loss of limb and life have been attributable to MDROs. . . . Given the continuing operational tempo of our overseas contingency operations, we can expect that injuries and infections with MDROs will continue in our facilities at all levels.”
— Witness Statement of Captain Gregory J. Martin, Medical Corps, United States Navy, and Judith English, Bureau of Medicine and Surgery, before the House Armed Services Subcommittee on Oversight and Investigations, September 29, 2010






