Antibiotic Stewardship Programs Vary in U.S. Hospitals
CDC survey explores how hospital size, location may influence details
This fact sheet was updated in September 2017 with 2015 antibiotic stewardship program survey data from CDC.
Overview
Up to 50 percent of antibiotic use in hospitals is considered inappropriate,1 which contributes to antibiotic resistance as well as other adverse events for patients. Hospitals have begun to address this misuse by implementing antibiotic stewardship programs (ASPs), which aim to ensure that these drugs are prescribed only when necessary, to improve antibiotic prescribing and patient safety. Implementing these programs in all inpatient facilities is a goal outlined in the National Action Plan for Combating Antibiotic-Resistant Bacteria.
In 2015, the Centers for Disease Control and Prevention (CDC) conducted a comprehensive evaluation of ASPs in 4,569 U.S. hospitals to determine how many included all seven of CDC’s core elements recommended for hospital antibiotic stewardship programs.2 These core elements are:
- Leadership commitment: Dedicating the necessary human, financial, and information technology resources to the program.
- Accountability: Appointing a leader who is responsible for program outcomes.
- Drug expertise: Identifying a pharmacist in charge of working to improve antibiotic use within an institution.
- Action: Implementing at least one practice or policy designed to improve prescribing.
- Tracking: Monitoring patterns of antibiotic prescribing and resistance within the institution.
- Reporting: Relaying information on antibiotic use and resistance within the institution on a regular basis to doctors, nurses, and other relevant staff.
- Education: Teaching the institution’s clinicians about antibiotic resistance and optimal prescribing habits.
The CDC found that just over 48 percent of the facilities had ASPs that included all seven core elements. Presented below are selected outcomes from this study that explore the association between hospital size, location, and the presence of specific core elements on stewardship programs.
ASPs by facility characteristics and region
Facility size was an important factor associated with the implementation of comprehensive stewardship programs. More larger institutions reported having all seven core elements in their ASPs—66 percent of hospitals with greater than 200 beds, compared with 50 percent of hospitals with 51 to 200 beds and 31 percent of hospitals with 50 or fewer beds. Similarly, a higher percentage of teaching facilities, which are typically larger than 200 beds, reported implementing all seven elements compared with nonteaching facilities. These findings underscore the importance of examining the resource gaps and barriers unique to smaller hospitals when establishing ASPs.
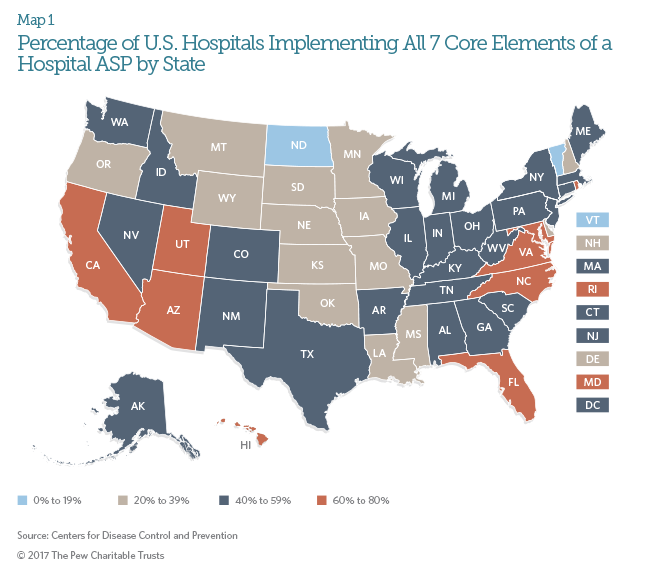
ASP implementation also varied by location. States with higher percentages of hospitals including all seven core elements were largely concentrated in the Northeast and West, with Utah having the highest percentage of facilities reporting all seven core elements. California, the only state with legislation that mandated ASPs in hospitals at the time of this study, had the second highest percentage of facilities reporting all seven core elements, highlighting the impact state policy can have on expanding ASP implementation.
Core elements of ASPs
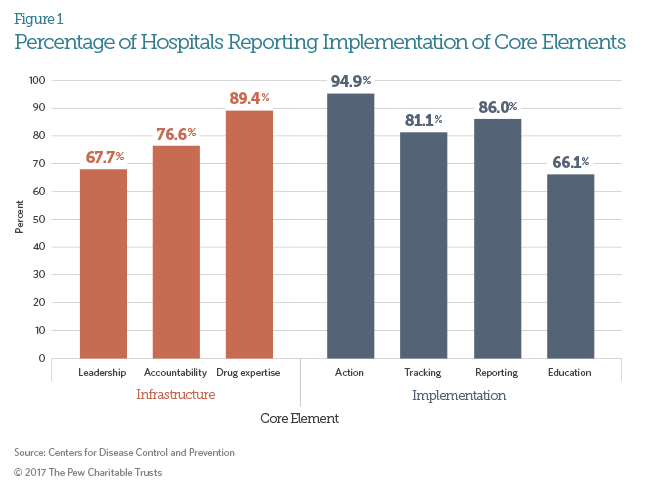
There was considerable variability in how frequently each core element was implemented by hospitals. (See Figure 1.)
Among all facility characteristics and core elements, leadership commitment was the strongest predictor for a hospital having a comprehensive ASP. Facilities that had written support from hospital administrators were six times more likely to have a stewardship program that included all seven core elements. Salary for staff to engage in stewardship was also significantly predictive of a comprehensive program. These results highlight the considerable impact that support from hospital leadership has on successful ASPs. Facilities with limited resources can consider establishing this core element first, before gradually adding components of an ASP.
In contrast, action was the most commonly implemented core element. Examples of action varied and included facility-specific treatment recommendations, which offer guidance for providers on appropriate antibiotic management for specific conditions, and antibiotic “timeouts,” during which clinicians reassess whether a patient’s antibiotic therapy should be continued or modified, generally 48 hours after beginning the therapy.3
Many hospitals have already begun implementing ASPs, driven in part by recent national policies that encourage stewardship programs for all inpatient facilities. Understanding the national variation in ASPs, whether by facility size, location, or program content, will provide key lessons for other facilities on how to successfully implement stewardship programs and reduce inappropriate antibiotic use.
Endnotes
- Amy L. Pakyz et al., “Trends in Antibacterial Use in US Academic Health Centers: 2002 to 2006,” Archives of Internal Medicine 168, no. 20 (2008): 2254–60, http://dx.doi.org/10.1001/archinte.168.20.2254; and Scott Fridkin et al., “Vital Signs: Improving Antibiotic Use Among Hospitalized Patients,” Morbidity and Mortality Weekly Report 63, no. 9 (2014): 194–200, http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6309a4.htm.
- Erin N. O’Leary et al., “Uptake of Antibiotic Stewardship Programs in U.S. Acute Care Hospitals: Findings From the 2015 National Healthcare Safety Network Annual Hospital Survey,” Clinical Infectious Diseases (2017): http://dx.doi.org/10.1093/cid/cix651.
- Lori A. Pollack et al., “Antibiotic Stewardship Programs in U.S. Acute Care Hospitals: Findings From the 2014 National Healthcare Safety Network Annual Hospital Survey,” Clinical Infectious Diseases 63, no. 4 (2016): 443–49, http://dx.doi.org/10.1093/cid/ciw323.