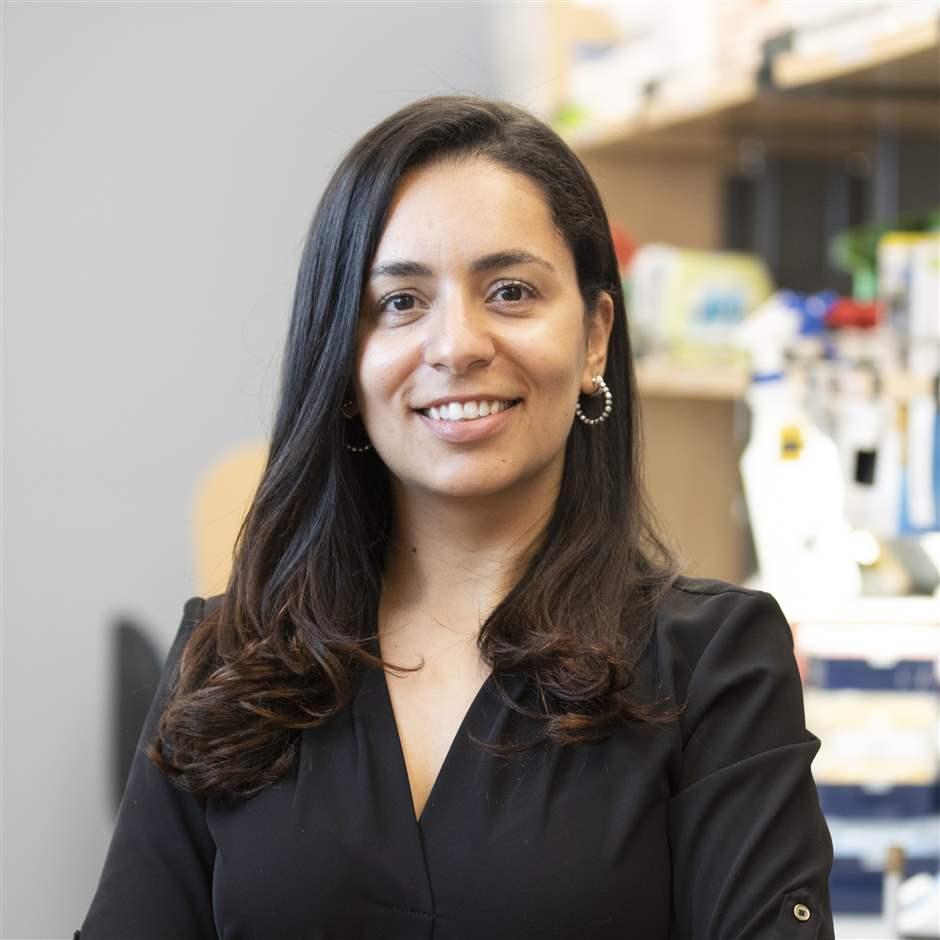
Pew Scholar Examines Disruptions to Early Microbiome Development
Dr. Mariana Byndloss is exploring the connection between antibiotic use, diet, and obesity during childhood

The array of microbes lining our intestines is critical to maintaining long-term health and wellness. Known as the gut microbiome, it supports everything from good digestion to a robust immune system.
This community of bacteria begins growing in infancy and continues throughout life. However, this process is not well understood, and several Pew biomedical scholars are searching for answers about what helps—and hinders—the development of a robust gut microbiome.
One of these scholars is Dr. Mariana Byndloss, an assistant professor at Vanderbilt University. Byndloss is researching how factors such as diet and antibiotic exposure during childhood can compromise the gut. Her work could offer new insights into how to better protect and heal the microbiome when things go awry.
This interview with Byndloss has been edited for length and clarity.
Tell us about the link between childhood antibiotic use and obesity.
We know that antibiotic use in early life can compromise the microbiome and become a risk for obesity and other diseases. Kids with more than one exposure to antibiotics, either through prescription medications or the food they eat, are at higher risk of having obesity later. And it seems that the earlier in life you get exposed to antibiotics, the greater the risk of consequences.
Are these changes to the microbiome permanent?
In our studies in mice, we found that as soon as you remove antibiotics, some of the microbiome is restored. However, there are still long-lasting effects that put the mice on a trajectory for obesity, especially if the animal is eating a western-style, high-fat diet.
Speaking of diet, what role does it play in childhood obesity?
In the past, researchers mostly focused on one risk factor for obesity: either antibiotic use or the western-style, high-fat diet. My lab is interested in the synergy between these two. For example, the parts of the country where kids are eating more fast food or a high-fat diet are also the areas where more antibiotics are prescribed. We think this combination of risk factors is altering the gut microbiome, so we want to find out what happens at a biological level when this occurs.
What, specifically, is your lab you looking at?
We’re interested in how the gut microbiome is talking to our intestines to prevent disease, and what happens when this beneficial crosstalk gets disrupted by factors such as a high-fat diet or antibiotics. In a recent study published in Cell Host & Microbe, our team was able to pinpoint which specific microbe was protecting the animals against obesity after antibiotic exposure.
How did you conduct the study?
When we administered antibiotics to mice, we found that the drugs were killing a specific microbe in the gut: a known probiotic called lactobacillus, which produces phenyllactic acid (PLA). We discovered that this metabolite was protecting the gut against obesity in mice without antibiotics. But when antibiotics were given, the drugs wiped out these lactobacillus microbes—and the intestinal epithelium (the cells lining the gut) produced excess fat, leading to obesity.
Is that irreversible, that loss of lactobacillus?
No, fortunately. Once antibiotics depleted the mouse’s gut microbes, we then reintroduced lactobacillus. And we found that even when a mouse had been given both antibiotics and a high-fat diet, receiving lactobacillus supplementation restored its ability to protect against obesity. We had the same results when we reintroduced PLA, the metabolite lactobacillus produces.
How might these findings be applied to human health and medicine?
Antibiotics are still an effective treatment for many infections. So, in situations where kids are prescribed a necessary antibiotic, our research shows that feeding them a healthy diet can help protect against some of these adverse effects. In a dream scenario, my lab would also love to someday see the metabolites we’ve identified—such as PLA—be used in place of dietary supplements like probiotics to further protect kids against the detrimental side effects of antibiotic use.