Antibiotic Use in Urgent Care Centers Shows Need for Improvement
Prescribing for many common conditions is higher than in other outpatient settings
Urgent care centers—outpatient facilities where patients seek immediate and unscheduled medical attention—play an important role in the fight against antibiotic resistance as outpatient care providers in the United States. Overuse of antibiotics can contribute to resistance, and improved use is critical to combating this public health threat. A new study from The Pew Charitable Trusts and the Centers for Disease Control and Prevention shows that antibiotic stewardship efforts are needed in urgent care centers to help reduce inappropriate prescribing.
Most antibiotic use in the U.S. health care system occurs in outpatient settings.1 Previous analysis by Pew and CDC found that nearly 1 in 3 antibiotics prescribed in physicians’ offices, emergency departments, and hospital specialty clinics was unnecessary.2 This brief focuses on urgent care centers.
What Are Urgent Care Centers?
Urgent care facilities—which are often open outside of regular business hours and diagnose and treat patients with common illnesses such as flu, colds, infections, and non-life-threatening injuries*—play a large role in providing outpatient care in the United States. Industry groups estimate that patients make over 160 million visits annually to these facilities.†
Urgent care centers differ from other outpatient facilities such as retail or office-based health clinics. Retail health clinics are walk-in facilities located within retail businesses—such as pharmacies, grocery stores, or drugstores—that are often staffed by nurse practitioners and physician assistants, and provide outpatient preventive and primary care services.‡ Office-based clinics are outpatient facilities other than hospitals, skilled nursing facilities, community health centers, military treatment facilities, intermediate care facilities, or state or public health clinics where primary care services are provided.§
* AMN Healthcare, “Convenient Care: Growth and Staffing Trends in Urgent Care and Retail Medicine” (2015), https://www.amnhealthcare.com/uploadedFiles/MainSite/Content/Healthcare_Industry_Insights/Industry_Research/AMN%2015%20W001_Convenient%20Care%20Whitepaper(1).pdf.
† Urgent Care Association of America, “Urgent Care Industry Information Kit” (2013), http://c.ymcdn.com/sites/www.ucaoa.org/resource/resmgr/Files/UrgentCareMediaKit_2013.pdf.
‡ RAND Corp., “The Evolving Role of Retail Clinics” (2016), http://www.rand.org/pubs/research_briefs/RB9491-2.html.
§ Centers for Medicare & Medicaid Services, “Place of Service Code Set,” accessed March 29, 2017. https://www.cms.gov/Medicare/Coding/place-of-service-codes/Place_of_Service_Code_Set.html.
New findings in the Journal of the American Medical Association Internal Medicine show that nearly 2 in 5 visits to urgent care centers in 2014 resulted in an antibiotic prescription. The majority of antibiotics prescribed in these settings were associated with diagnoses of acute respiratory conditions for which antibiotics are often not recommended. This brief presents other key findings from this research.
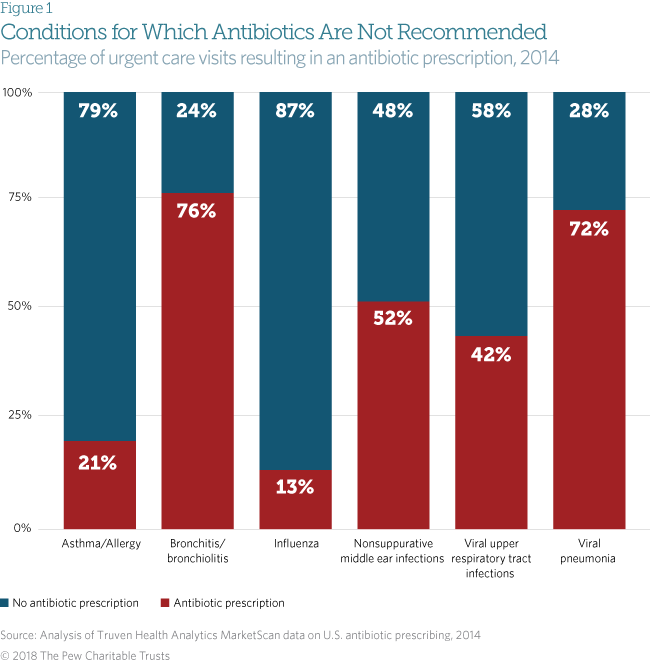
Conditions for which antibiotics are not recommended
National treatment guidelines do not recommend antibiotic use for several acute respiratory conditions, including viral upper respiratory tract infections (common cold), bronchitis/bronchiolitis, asthma/allergy, influenza, nonsuppurative middle ear infections (characterized by non-infected fluid in the middle ear), and viral pneumonia.3 Because these conditions are either caused by viruses or are noninfectious, antibiotics are not effective.
Yet about 46 percent of all urgent care visits for non-antibiotic recommended diagnoses resulted in an antibiotic prescription. This is comparatively higher than other outpatient health care settings, such as retail clinics, emergency departments, and office-based clinics – where the same visits ended with a prescription some 14, 25, and 17 percent of the time, respectively.
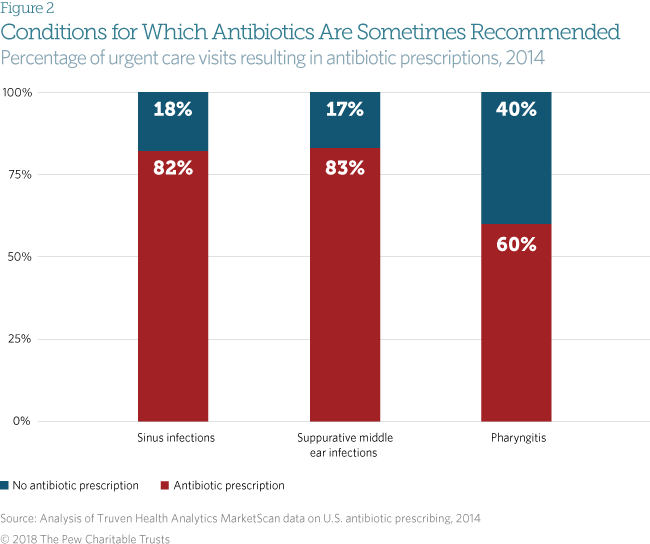
Conditions for which antibiotics are sometimes recommended
This study found high levels of prescribing for three common diagnoses:
- 82 percent of sinus infections treated in urgent care centers resulted in an antibiotic prescription, compared with 68 percent in emergency departments and 76 percent in office-based clinics.
- 83 percent of suppurative middle ear infections treated in urgent care centers resulted in an antibiotic prescription, compared with 72 percent in emergency departments and 79 percent in office-based clinics.
- 60 percent of pharyngitis (inflammation of the throat) cases treated in urgent care centers resulted in an antibiotic prescription, compared with 47 percent in emergency departments and 51 percent in office-based clinics.
Antibiotic use is not always recommended for patients with these three conditions. Some of these patients may improve without antibiotic treatment, while other cases can be caused by viruses and thus do not respond to antibiotics. Some antibiotic prescribing for these conditions may be unnecessary, and increased stewardship efforts within urgent care centers are needed to ensure that antibiotics are prescribed for these diagnoses only when needed.
Methodology
This study was based on medical and pharmaceutical claims data from the Truven Health Analytics MarketScan commercial claims and encounters database, which captures individuals younger than 65 with employer-sponsored health insurance. Visits to urgent care clinics were matched with pharmaceutical claims for antibiotics within three days of the clinic visit in order to determine how many visits resulted in antibiotic prescriptions.
A tiered analytic strategy (described in a previous study)4 was used to link prescriptions with the most antibiotic-appropriate diagnosis a patient received during the associated urgent care visit. For example, if a patient was diagnosed with both bronchitis (a condition that does not warrant antibiotic treatment) and bacterial pneumonia (a condition that does require antibiotic use), the prescription was linked to the pneumonia diagnosis.
Limitations
This analysis has a number of limitations. For example, the number of visits to urgent care captured by this database is small compared with the anticipated number of visits to these facilities. This may be due to both the population included in the MarketScan database and the fact that not all urgent care centers necessarily file claims using the same facility code (which was used to identify urgent care visits in this analysis). For example, some urgent care centers may file claims using a primary care facility code and therefore would not be captured in this analysis.
The MarketScan data do not include Medicaid or Medicare patients, individuals covered by private insurance not provided through an employer, and patients who paid cash for the visit rather than file an insurance claim. This limits the ability to generalize these data.
Additional details on study limitations can be found in Journal of the American Medical Association Internal Medicine.5
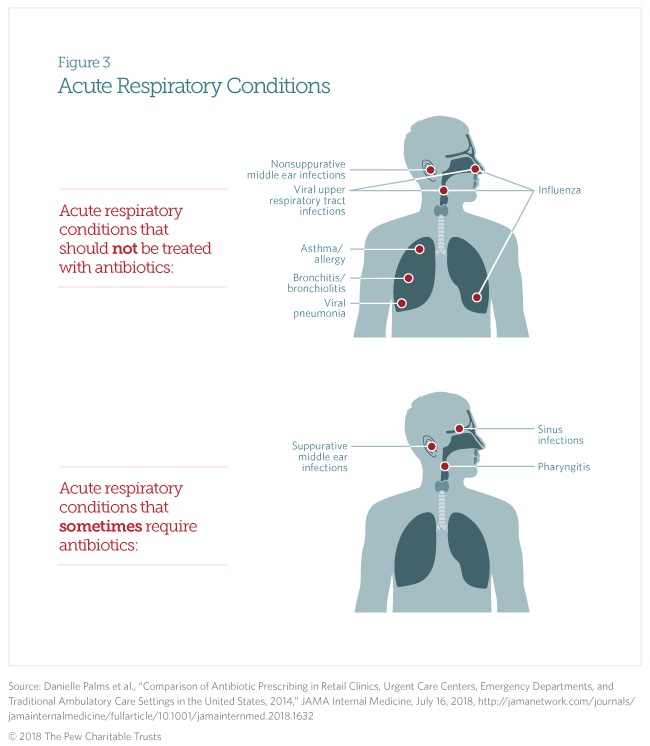
Acute Respiratory Conditions
Acute respiratory conditions include:
- Sinus infections.
- Middle ear infections.
- Pharyngitis.
- Viral upper respiratory conditions (common cold).
- Bronchitis and bronchiolitis.
- Asthma and allergy.
- Influenza.
- Pneumonia.
Sinus infections can be caused by both bacterial and viral pathogens. Treatment guidelines recommend antibiotic use only when the infection is suspected to be caused by bacteria,* a determination often based on clinical criteria such as whether the patient has experienced related symptoms for 10 or more days without improvement.
Suppurative middle ear infections are identified by the presence of pus. Pediatric guidelines recommend either treating patients with an antibiotic or, for certain patients, waiting 48 to 72 hours to see whether symptoms improve.†
Pharyngitis is a diagnosis of inflammation of the throat, which patients typically report as a sore throat. Treatment guidelines state that antibiotics should be prescribed only when the condition is caused by group A Streptococcus (strep throat),‡ an infection that can be confirmed through the use of a diagnostic test. Evidence suggests that approximately 37 percent of children and 18 percent of adults with pharyngitis have strep throat and require antibiotics.§
* Anthony W. Chow et al., “Executive Summary: IDSA Clinical Practice Guideline for Acute Bacterial Rhinosinusitis in Children and Adults,” Clinical Infectious Diseases 54, no. 8 (2012): e72–e112, http://dx.doi.org/10.1093/cid/cir1043; Richard M. Rosenfeld et al., “Clinical Practice Guideline (Update): Adult Sinusitis,” Otolaryngology–Head and Neck Surgery 152, suppl. 2 (2015): S1–S39, http://dx.doi.org/10.1177/0194599815572097; Ellen R. Wald et al., “Clinical Practice Guideline for the Diagnosis and Management of Acute Bacterial Sinusitis in Children Aged 1 to 18 Years,” Pediatrics 132, no. 1 (2013): e262–e280, http://dx.doi.org/10.1542/peds.2013-1071.
† Allan S. Lieberthal et al., “The Diagnosis and Management of Acute Otitis Media,” Pediatrics 131, no. 3 (2013): e964–e999, http://dx.doi.org/10.1542/peds.2012-3488.
‡ Stanford T. Shulman et al., “Clinical Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis: 2012 Update by the Infectious Diseases Society of America,” Clinical Infectious Diseases 55, no. 10 (2012): e86–e102, http://dx.doi.org/10.1093/cid/cis629.
§ Nader Shaikh, Erica Leonard, and Judith M. Martin, “Prevalence of Streptococcal Pharyngitis and Streptococcal Carriage in Children: A Meta-Analysis,” Pediatrics 126, no. 3 (2010): e557–e564, http://dx.doi.org/10.1542/peds.2009-2648; Andrew M. Fine, Victor Nizet, and Kenneth D. Mandl, “Large-Scale Validation of the Centor and McIsaac Scores to Predict Group A Streptococcal Pharyngitis,” Archives of Internal Medicine 172, no. 11 (2012): 847–52, http://dx.doi.org/10.1001/archinternmed.2012.950.
Acknowledgments
The project team—Kathy Talkington, David Hyun, Rachel Zetts, and Andrea Stoesz—would like to thank the Centers for Disease Control and Prevention, specifically Lauri Hicks, Katherine Fleming-Dutra, and Danielle Palms, for partnering with Pew on this work. Additionally, the team would like to thank Pew colleagues Heather Cable, Katherine Portnoy, Amelia Murphy, and Demetra Aposporos for their assistance in developing this brief.
Endnotes
- Katie J. Suda et al., “A National Evaluation of Antibiotic Expenditures by Healthcare Setting in the United States, 2009,” Journal of Antimicrobial Chemotherapy 68, no. 3 (2013): 715–18, http://dx.doi.org/10.1093/jac/dks445.
- Katherine Fleming-Dutra et al., “Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011,” Journal of the American Medical Association 315, no. 17 (2016): 1864–73, http://dx.doi.org/10.1001/jama.2016.4151; The Pew Charitable Trusts, ”Antibiotic Use in Outpatient Settings: Health Experts Create National Targets to Reduce Unnecessary Antibiotic Prescriptions” (2016), http://www.pewtrusts.org/~/media/assets/2016/05/antibioticuseinoutpatientsettings.pdf.
- Adam L. Hersh et al., “Principles of Judicious Antibiotic Prescribing for Upper Respiratory Tract Infections in Pediatrics,” Pediatrics 132, no. 6 (2013): 1146–54, http://dx.doi.org/10.1542/peds.2013-3260; Vincenza Snow, Christel Mottur-Pilson, and Ralph Gonzales, “Principles of Appropriate Antibiotic Use for Treatment of Nonspecific Upper Respiratory Tract Infections in Adults,” Annals of Internal Medicine 134, no. 6 (2001): 487–89, http://dx.doi.org/10.7326/0003-4819-134-6-200103200-00014; Scott F. Dowell et al., “Appropriate Use of Antibiotics for URIs in Children: Part II. Cough, Pharyngitis and the Common Cold,” American Family Physician 58, no. 6 (1998): 1335–42, http://www.aafp.org/afp/1998/1015/p1335.html; Shawn L. Ralston et al., “Clinical Practice Guideline: The Diagnosis, Management, and Prevention of Bronchiolitis,” Pediatrics 134, no. 5 (2014): e1474–e1502, http://dx.doi.org/10.1542/peds.2014-2742; Vincenza Snow, Christel Mottur-Pilson, and Ralph Gonzales, “Principles of Appropriate Antibiotic Use of Acute Bronchitis in Adults,” Annals of Internal Medicine 134, no. 6 (2001): 518–20, http://dx.doi.org/10.7326/0003-4819-134-6-200103200-00020; National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program, “Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma” (2007), http://www.nhlbi.nih.gov/files/docs/guidelines/asthgdln.pdf; Anthony E. Fiore et al., “Antiviral Agents for the Treatment and Chemoprophylaxis of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP),” Morbidity and Mortality Weekly Report 60, no. 1 (2011): 1–25, http://www.cdc.gov/mmwr/pdf/rr/rr6001.pdf; John S. Bradley et al., “Executive Summary: The Management of Community-Acquired Pneumonia in Infants and Children Older Than 3 Months of Age: Clinical Practice Guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America,” Clinical Infectious Diseases 53, no. 7 (2011): 617–30, http://dx.doi.org/10.1093/cid/cir625; Lionel A. Mandell et al., “Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults,” Clinical Infectious Diseases 44, suppl. 2 (2007): S27–S72, https://doi.org/10.1086/511159; American Academy of Family Physicians, American Academy of Otolaryngology—Head and Neck Surgery, and American Academy of Pediatrics Subcommittee on Otitis Media With Effusion, “Otitis Media With Effusion,” Pediatrics 113, no. 5 (2004): 1412–29, http://pediatrics.aappublications.org/content/113/5/1412.
- Fleming-Dutra et al., “Prevalence of Inappropriate Antibiotic Prescriptions.”
- Comparison of Antibiotic Prescribing in Retail Clinics, Urgent Care Centers, Emergency Departments, and Traditional Ambulatory Care Settings in the United States, 2014,” JAMA Internal Medicine, July 16, 2018, http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2018.1632.