Federal Provision Protects Patients Who Take Compounded Drugs From Another State
Law directs FDA and states to create incentives for safer drugs
Editor's note: This fact sheet was updated on June 26, 2018, to improve the headline’s clarity.
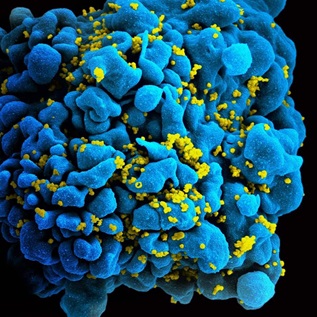
Contaminated and improperly stored injectable products from a Massachusetts-licensed compounding pharmacy caused a fungal meningitis outbreak in 2012 that killed dozens of people and injured hundreds more. Notably, while patients were harmed in 20 states, none lived in Massachusetts, where the pharmacy was located.
In response to this tragedy, Congress enacted the Drug Quality and Security Act (DQSA), reinvigorating the Food and Drug Administration’s (FDA’s) compounding regulatory program. One important component of the law is a provision directing FDA to set rules for shipment of compounded drugs over state lines.1 Robust implementation and enforcement of this provision is critical to ensuring that patients in a given state are protected when receiving drugs produced by a pharmacy in another state.
Compounded drugs are produced by, or under the oversight of, pharmacists or physicians rather than drug manufacturers. They are typically created to meet a patient’s medical needs when a commercially available, FDAapproved product cannot. For example, a young child who needs a liquid version of a medicine that is approved only in pill form, or a seizure patient on a sugar-free diet who needs a drug that, in its approved form, has sugary flavoring, could get compounded versions of the medications they need.
The vast majority of compounded drugs come from traditional compounders—pharmacies or physicians who distribute or dispense drugs to individual patients, after receiving a prescription, for administration at home or in a doctor’s office.2 Traditional compounders are overseen by the state in which they are located, and each state has its own oversight system for these practitioners and their facilities.
Although many traditional compounders exclusively serve patients in their own state, others dispense products to patients elsewhere in the country. Such interstate activity can range from small-scale local distribution (for example, a compounder located at a state border dispensing to the neighboring community) to businesses that operate at a significant scale sending products nationwide. As an example of the latter, some patients who cannot eat and digest normally require intravenous administration of liquid nutrition that is tailored to their individual dietary needs. Those infusions are often prepared by specialized compounders who may be located across the country from the patient. Other compounders may advertise compounded products online and thus receive orders from around the country.
Because traditional compounders can and do ship products across state lines, patients everywhere can be put at risk if any state has ineffective oversight. Federal law addresses this risk by offering states a choice: They may choose to enter into a memorandum of understanding (MOU) with FDA committing to certain oversight functions, after which pharmacies in those states may distribute a larger percentage of their compounded products interstate than may pharmacies located in states that do not sign the MOU.3 Traditional compounders in states that do not sign the MOU are limited to distributing no more than 5 percent of their products interstate, limiting these compounders largely to in-state sales.
The MOU provision of the DQSA is a critical safeguard to ensure appropriate oversight over compounded medications that are shipped across state lines. It helps to prevent compounders from setting up shop in a state with relatively weak oversight and then sending large quantities of drugs all over the country. Compounders in states that commit to respond to complaints about drugs shipped out of the state, as outlined in the MOU, will be able to sell more product interstate than will those in states that have not made such commitments. Therefore, the MOU provision creates an incentive for states to mitigate the risks of compounding, even if the patients at risk are out of state. And it encourages compounders who wish to do substantial business across state lines to locate in states whose oversight schemes are robust enough to protect patients in other states from poor-quality compounded drugs. The MOU provision is one way that the federal statute creates incentives for compounders to meet higher-quality standards, which translate into safer drugs.
Endnotes
- In the Drug Quality and Security Act, Congress removed uncertainty about the validity of Section 503A by excising the advertising provisions in that law that had been found to be unconstitutional. Congress otherwise left Section 503A intact, including the requirement for drugs to be compounded based on the receipt of a valid patient-specific prescription, and limitations on interstate distribution and dispensing of compounded drugs.
- Federal law does not use the term “traditional compounders”; the term is used here for clarity to describe entities regulated under Section 503A of the Federal Food, Drug, and Cosmetic Act.
- Food, Drug, and Cosmetic Act of 1938, 21 U.S.C. § 353(a)(b)(3)(B) (1938); and Food and Drug Administration Compliance Policy Guide, Pharmacy Compounding, Sec. 7132.16 (1992). This concept first arose in the Food and Drug Administration’s 1992 Compliance Policy Guide, which listed “distributing inordinate amounts of compounded products out of state” as one of the activities FDA would consider in determining whether the activities of a pharmacy raised “the kind of concerns normally associated with a manufacturer.” The concept was incorporated in the federal statute in 1997 and retained when the statute was reaffirmed in 2013.


Quality Standards for Stock Supplies of Compounded Drugs Keep Patients Safe
Federal law ensures that compounders meet requirements to reduce public health risks
State Oversight of Drug Compounding
Major progress since 2015, but opportunities remain to better protect patients