LPAD: A Regulatory Pathway to Develop Antibiotics and Fight Drug-Resistant Infections
This Q&A has been updated. Read A New Way to Approve Antibiotics for Drug-Resistant Infections.
The Antibiotic Development to Advance Patient Treatment (ADAPT) Act, originally introduced in 2013, was recently included as part of the 21st Century Cures Act, the wide-ranging health care bill approved by the House Energy and Commerce Committee on May 21. ADAPT, along with companion legislation in the Senate (the Promise for Antibiotics and Therapeutics for Health, or PATH, Act) would require the Food and Drug Administration to establish a new approval process known as the Limited-Population Antibacterial Drug pathway, or LPAD.
Why is an alternate regulatory pathway needed for limited-population antibacterial drugs?
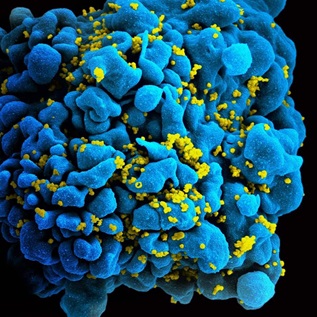
Antibiotic resistance is on the rise. More than half of infectious disease doctors surveyed have cared for a patient with an infection resistant to all available antibiotics.1
The Centers for Disease Control and Prevention recently emphasized the risk of losing effective antibiotics—which would not only limit the ability to fight routine infections but also erode the ability to safely perform surgery, treat cancer and rheumatoid arthritis, and provide kidney dialysis and organ transplants.2
As FDA acknowledges, it is difficult to identify patients suffering from highly resistant bacterial infections and enroll them in sufficient numbers for traditional, large-scale clinical trials because only a small number of patients are diagnosed with these serious conditions. An LPAD would allow smaller clinical studies and should help make antibiotic development more feasible—scientifically and financially.
What would LPAD do?
LPAD would allow FDA to approve new antibiotics and antifungal drugs that address unmet medical needs for limited populations of patients. Antibiotics approved under this pathway would target serious or life-threatening infections for which few or no suitable options exist and would be studied for use in smaller populations than antibiotics used for broader indications or conditions.
To ensure that LPAD-approved drugs are used only for the intended patients, these drugs would bear labels indicating the limited population for which they are appropriate. FDA would have the authority to review promotional materials before a drug company could use them for marketing and would mandate evaluation of how antibiotics approved under this pathway were prescribed.
What types of studies would be required for the approval of antibiotics under this pathway?
FDA would have the flexibility to consider a variety of evidence in determining whether to approve antibiotics for limited populations, but it would not mandate that particular data be submitted. In general, FDA regulations do not specify the level of evidence needed to support approval of a drug. Instead the agency develops, publishes, and updates guidance documents that assist drugmakers in planning clinical development programs for new antibiotics. The agency recently issued draft guidance on the development of antibacterial therapies for patients with unmet medical needs.
Is LPAD an expedited pathway or accelerated approval?
While products developed under LPAD would still be eligible for existing expedited FDA pathways (such as fast track, breakthrough therapy, accelerated approval, and priority review), LPAD would not guarantee a shorter review time by the agency. Nor does LPAD specify use of a “surrogate endpoint” as a proxy for a patient’s clinical response as under the accelerated approval pathway described in 506(c) of the Federal Food, Drug, and Cosmetic Act . However, drugs approved under this pathway may take less time to develop because clinical studies are likely to be smaller than those conducted for approval of drugs for broader use.
Would LPAD lower the safety and efficacy standards needed for FDA approval?
Drugs approved under the pathway would have to meet the same safety and efficacy standards as any other drug under existing law.
Every approved drug is meant to treat a specific population, and the benefit-risk calculation for patients lacking other treatment options is different from that of broader populations with easily treatable infections.
The FDA would consider benefits and risks for the sickest patients with few or no available treatment options whose level of acceptable risk is different from those with readily available treatment options. LPAD’s labeling and marketing provisions would help reduce the likelihood that these drugs would be used in populations that could be adequately treated with therapies approved for a broader population.
Why is LPAD needed in addition to the Generating Antibiotic Incentives Now (GAIN) Act?
The two approaches are complementary. GAIN is a 2012 law that provides an economic incentive to drugmakers that bring new antibiotics for serious infections to market. In contrast, LPAD helps streamline the regulatory process for antibiotics and makes it more feasible for drugmakers to test antibiotics for patients that need them most and to obtain FDA approval.
What ensures that LPAD drugs would be used as intended?
LPAD would not limit a physician’s ability to choose the most appropriate drug, but the bill contains several important provisions to reduce the likelihood that limited-population drugs would be used broadly. A limited-population designation comes with mandatory labeling that communicates to physicians and other health care providers that these antibiotics were demonstrated to be safe and effective only in limited populations.
In addition to the designation requirements already in the bill, Pew is advocating for labeling with prominent language or other visual elements that make the approved uses of these drugs immediately clear.
FDA would have the authority to review promotional materials before distribution and require monitoring of the usage of antibiotics approved under this pathway.
Endnotes
- Adam L. Hersh et al., “Unmet Medical Need in Infectious Diseases,” Clinical Infectious Diseases (2012), doi:10.1093/cid/cis275.
- Centers for Disease Control and Prevention, “Antibiotic Resistance Threats to the United States, 2013,” http://www.cdc.gov/drugresistance/threat-report-2013/index.html.