COVID-19 Tests Highlight Need for Strengthened FDA Oversight and Diagnostics Legislation
Reforms would ensure rigorous, efficient reviews of test accuracy

Overview
The COVID-19 pandemic created overwhelming demand for tests that diagnose the disease or identify past infection. The U.S. Food and Drug Administration (FDA) has responded by authorizing the emergency use of more than 300 coronavirus tests that medical device manufacturers and laboratories have developed to meet the varying needs of health care providers and public health authorities.1
This brief examines FDA oversight of COVID-19 tests and how events during the pandemic reinforce the need for legislation—such as the bipartisan Verifying Accurate Leading-Edge IVCT Development (VALID) Act—that would improve regulation of all in vitro clinical tests (IVCTs). Also called in vitro diagnostics (IVDs), these tests analyze samples from the human body such as blood, mucus, and saliva and are among the most widely used tools in medicine. Their results guide diagnosis and treatment of cancer, genetic disorders, and hundreds of infectious diseases, including COVID-19.
FDA oversight of diagnostic tests is critical to protecting patients and public health. For example, in January 2021, FDA warned that Curative Inc.’s SARS-CoV-2 test, a COVID-19 diagnostic, presented a risk of false results, particularly false negatives, when not used according to its authorized labeling, which advises performing the test on symptomatic individuals within 14 days of symptom onset, under a health care worker’s direct supervision. The agency emphasized the importance of following these guidelines and recommended that test administrators consider retesting individuals if a recent inaccurate result was suspected, as failure to adhere to the guidelines could increase the risk that infected people do not receive appropriate treatment and unknowingly spread the disease to others.2 At the time of FDA’s announcement, clinicians were administering the test nearly a million times per week, often on asymptomatic people including residents of Chicago, Houston, and Los Angeles; personnel at military facilities; members of Congress; and Capitol Hill staff.3
Despite the public health benefits of the agency’s oversight, tests developed and used within a single laboratory are generally not required to undergo FDA review, nor does the agency always know which of these lab developed tests (LDTs) are being used on patients. However, during public health emergencies, the agency has generally required all developers—including both device companies and labs—to apply for emergency use authorizations (EUAs) for any test marketed to diagnose or screen for the disease that is the subject of the declared emergency. This allows FDA to know which diagnostics are entering the market, conduct risk-based reviews of their accuracy and reliability, monitor their performance, and, when necessary, amend or revoke a test’s EUA in response to new information.
FDA should have such fundamental regulatory tools for all IVDs, no matter where they are made and used, and whether or not there’s a pandemic. A legislative solution is needed to ensure the agency has these authorities, particularly in light of a Department of Health and Human Services (HHS) decision in 2020 that undermined oversight of LDTs even during a public health emergency.4 According to the HHS statement, FDA would not be able to require makers of LDTs to submit their products for review before using them on patients unless the agency first went through a lengthy rule-making process. This policy could lead to test accuracy problems, with potentially significant consequences for patient health, especially during an already dangerous pandemic.
HHS’s decision to limit FDA’s emergency oversight powers demonstrates why lawmakers should act to strengthen the agency’s review of the growing market for diagnostic tests. Congress should pass reforms that would create a flexible and risk-based FDA oversight system, while also preserving the EUA powers that FDA effectively used to expand COVID-19 testing capacity. The most comprehensive legislative proposal to address such reforms is the bipartisan VALID Act, which would unify regulation of all diagnostic tests and help level the playing field for the companies and labs creating these important products. Although the measure needs a few key improvements—including strengthening FDA’s postmarket powers and narrowing the bill’s criteria for tests that would be excluded from premarket review requirements—it is a strong start to creating a risk-based review system that delivers reliable IVDs for patients.5


Test Regulation Should Rank High on Agenda of Congress
The role of FDA in regulating COVID-19 tests
Following then-HHS Secretary Alex Azar’s declaration of a public health emergency on Jan. 31, 2020, FDA announced that, under the Pandemic and All Hazards Preparedness Act, the agency would need to grant an EUA to any test marketed to diagnose or screen for COVID-19, as had been the case in prior emergencies. An EUA temporarily allows makers of a specific FDA-regulated product—including diagnostic tests—to market these items without completing the agency’s standard safety and efficacy review process. This flexibility lets the agency make products available quickly in an emergency while still ensuring that their known and potential benefits outweigh their risks.6
The emergency powers granted to the agency during a pandemic also allow it to amend or revoke authorizations as it learns more about a product’s safety, effectiveness, or performance in the field. Through this process, FDA can move quickly to issue a safety warning or recall a product when subsequent evidence reveals that it is ineffective, unreliable, or has a safety issue.
Until August 2020, both test kits developed by device manufacturers and LDTs were required to receive an EUA. In order to speed access to testing, the agency also allowed test developers—including laboratories—to bring a test to market immediately, provided that the developer validated the test for accuracy prior to its use on patients, notified FDA of its intent to offer the test, and submitted an EUA request within 15 days of that notification. The agency could then follow up as necessary to ensure that the tests met the authorization standards. This follow-up was critical: When the agency subsequently reviewed a sample of the EUA applications that came from labs, it found that nearly two-thirds of them had design or validation issues that needed to be addressed before the tests could be authorized. FDA was able to work with many of these developers to help correct the initial problems.7
Tests developed for COVID-19 and their roles during the pandemic
FDA was able to use its EUA flexibility to ensure a variety of tests reached the market during the pandemic. (See Table 1.) This is critical given the scale of the need and the many different types of settings in which testing may be carried out.
The authorized tests for COVID-19 can be grouped into two main categories, depending on their intended use: diagnostic tests and antibody tests. Diagnostic tests identify active COVID-19 infection using samples collected from a patient’s respiratory system—either through a nasopharyngeal, nasal, or throat swab—or from a saliva sample. Clinicians can then refer patients who test positive for treatment or isolation to protect others and mitigate spread of the virus. Thus far, two main types of diagnostic tests have been developed: molecular tests, which detect the presence of the virus’s genetic material; and antigen tests, which detect the presence of specific proteins on the virus’s surface.8
Antibody tests, on the other hand, use a blood sample to determine whether a patient was previously infected with the virus.9 While antibody tests cannot diagnose or rule out a current COVID-19 infection, they serve an important public health role in measuring exposure within communities and mapping outbreaks.
Table 1
FDA Oversight Ensures Different Types of COVID-19 Tests Can Be Developed
| Traditional molecular | Rapid molecular | Antigen | Antibody | |
|---|---|---|---|---|
| Purpose | Diagnose active infection | Identify past infection | ||
| Specimen type10 | Nasopharyngeal, nasal, or throat swab; saliva | Nasopharyngeal, nasal, or throat swab; saliva | Nasopharyngeal or nasal swab; saliva | Blood (from finger stick or blood draw) |
| What is test detecting?11 | Viral RNA | Viral RNA | Viral proteins | Antibodies specific to SARS-CoV-2 |
| Pros | The most widely used molecular test, reverse transcription polymerase chain reaction (RT-PCR), is considered the “gold standard” in terms of accuracy.12 RT-PCR tests are used to detect the virus’s genetic material. |
Quicker to run compared with traditional molecular tests (approximately one hour or less).13 Can be done at the point of care (POC). In addition, the first test authorized for at-home use provides results within 30 minutes.14 Can identify those exposed to COVID-19 about a day sooner during the course of infection compared with a rapid antigen test.15 |
Can get results in less than 30 minutes.16 Can be done at POC, such as a hospital, clinic, or home care setting. In addition, at least one test is authorized for at-home use without the need for a prescription.17 |
Some tests can be done at POC with results in less than 30 minutes.18 |
| Cons | RT-PCR can take several hours to run and requires expensive equipment operated by trained personnel. Furthermore, backlogs and specimen transport to lab can delay results by several days.19 |
Not as accurate as laboratory-based molecular tests.20 May not be widely available in some areas.21 |
More likely to miss active infection compared with molecular tests. Sensitivity can be as low as 80%.22 |
Cannot diagnose active infection.23 Accuracy can vary depending on test type and when it is performed.24 |
| Use in the pandemic | Generally, the most accurate test type to confirm active infection. | Enable increased testing capacity since they can be performed relatively quickly at POC or at home. They serve as an important supplementary tool to traditional RT-PCR tests, especially for populations that may need repeated screening or don’t live near specialized labs. | Enable increased testing capacity since they can be performed relatively quickly at POC or at home. They serve as an important supplementary tool to RT-PCR tests, especially for populations that may need repeated screening or don’t live near specialized labs. | Aid in disease surveillance to inform public health strategies. They are an important tool to understanding disease prevalence. Can potentially be used to understand false positive/negative rates of diagnostic tests. |
| Examples of FDA oversight actions during the pandemic | FDA issued an announcement about the risk of false results, particularly false negatives, with the Curative SARS-CoV-2 test.25 | FDA revised the EUA for the Abbott ID Now Point-of-Care Test to provide additional guidance on how the test should be used to ensure accuracy and reliability.26 | FDA issued a safety announcement stating that false positive results can occur with antigen tests.27 | FDA revoked the EUA for a Chembio antibody test due to concerns with its accuracy.28 (See below for more information.) |
COVID-19 tests can vary in terms of how they are conducted, their accuracy, and their cost. For example, the more accurate and time-consuming laboratory-based molecular tests can cost hospitals and insurers $150 per test, while the less accurate and speedier antigen costs can cost as little as $5.29 The first authorized at-home test is expected to cost $50.30
The variety of COVID-19 tests underscores the value of EUA flexibility and shows that risk-based FDA oversight is compatible with getting innovative products to market.
What factors affect a test’s performance?
FDA serves an important role by establishing minimum standards for test performance, ensuring tests are labeled appropriately, and removing unreliable ones from the market. The accuracy of any test depends on factors including sensitivity, specificity, and disease prevalence within a population.
Sensitivity refers to the ability of a test to accurately identify patients with a disease or medical condition. In a group of 100 positive patients, a test that is 95% sensitive will be able to correctly identify 95 of those patients as positive. The other five patients will falsely test negative. Specificity, on the other hand, refers to the ability of a test to accurately identify patients without a disease or medical condition. In a group of 100 negative patients, a test that is 95% specific will be able to correctly identify 95 of those patients as negative. The other five patients will falsely test positive.31
It is important to note that sensitivity and specificity refer to the inherent properties of a test, and do not consider actual disease prevalence within a population.32 Although a test with 90% sensitivity and 90% specificity seems highly accurate, in a population where only a small number of patients are infected, the false negative and false positive rate may actually be much higher. For example, consider 100 college students where the actual prevalence of COVID-19 is 10%—meaning 10 students are infected. If all were tested with a product that is 90% sensitive and 90% specific, the results would include:
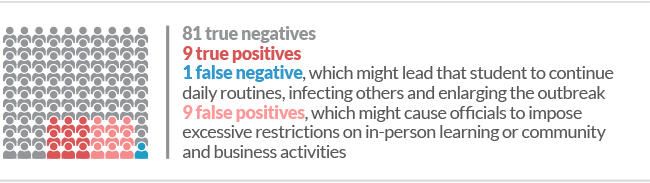
Therefore, it is also useful to consider each test’s predictive value, which heavily depends on disease prevalence within a given population.33 The positive predictive value (PPV) refers to the likelihood that a patient with a positive test result is truly positive,34 whereas the negative predictive value (NPV) refers to the likelihood that a patient with a negative result is truly negative.35 In the example above, the PPV (likelihood that a college student receiving a positive result is actually positive) would only be about 50%. With increasing disease prevalence in a population, the PPV will increase and the NPV will decrease.36
The need for legislative reform
Some test developers argue that FDA does not have jurisdiction over LDTs because the tests are tools used in the practice of medicine, which the agency does not regulate. However, FDA contends that diagnostics are medical devices that fall under the agency’s oversight through the Medical Device Amendments of 1976. At the time of that bill’s passage, LDTs were relatively simple and low-risk, often used for rare diseases or relying on manual interpretation. As a result, these tests were not typically subjected to the more stringent regulatory requirements that apply to other IVDs. Over the years, as LDTs have become more complex, FDA has attempted to exert more oversight over them, issuing warning letters to labs in cases where it became aware of flawed tests.
During the COVID-19 pandemic, FDA has taken numerous actions to protect public health and communicate concerns about potentially unreliable tests. For instance, in the case of Chembio’s SARS-CoV-2 antibody test, which was one of the first tests authorized by FDA, the agency reviewed data submitted by Chembio, as well as an independent evaluation at the National Institutes of Health’s National Cancer Institute, and found that the test generated a higher rate of false results than originally expected or reflected in its authorized labeling. As a result, FDA revoked the test’s EUA.37 FDA was able to conduct such reviews and take necessary action due to the emergency powers it enforced during the pandemic—powers it generally does not exercise over LDTs outside of a public health emergency.
However, in August 2020, HHS announced that—even during a public health emergency—FDA would not require LDT developers to submit their products for premarket review until the agency goes through formal rule-making,38 a process that often takes years. This decision means that makers of any new LDT—for diagnosing COVID-19 or other conditions such as high cholesterol, diabetes, and cancer—do not need FDA review to ensure the accuracy of their products. Even when expedited through the EUA process, FDA review provides an important check to ensure that health care providers and patients can trust a test’s results. This quality assurance is important, especially in a pandemic. FDA recently reviewed 125 EUA applications for COVID-19 tests from labs and found that 82 of them had design or validation problems that needed to be addressed before they could be authorized.39
The HHS decision also casts doubt on FDA’s ability to protect patients if it does learn of a faulty LDT on the market. The initial announcement did not specify whether FDA’s other regulatory authorities for diagnostics— such as the power to conduct lab inspections or recall tests—were still in effect. HHS subsequently said that LDTs remain subject to FDA regulation under the Public Health Services Act. Still, because most of the agency’s authority over diagnostic tests stems from the Food, Drug, and Cosmetic Act, FDA’s power to regulate LDTs remains unclear.
In addition to undermining critical public health protections, this decision by HHS has created confusion for test developers trying to understand how tests will be regulated. It is also unlikely to create much additional testing capacity, as tests without an EUA are not eligible for liability protection under the Public Readiness and Emergency Preparedness Act, and may have more trouble receiving reimbursement.
The decision highlights the need for overarching reform to close the gaps in the current fragmented diagnostics regulatory system. One proposal that aims to address the issue is the bipartisan VALID Act, which would give FDA clear authority to set risk-based requirements for all tests, including LDTs. Any legislative solution— including the VALID Act, which is expected to be reintroduced in 2021—should maintain FDA’s central role in overseeing diagnostic tests, and should ensure that they are held to the appropriate risk-based standards for quality, accuracy, and reliability—regardless of where they are developed and used.
Conclusion
Over the past year, the COVID-19 pandemic has underscored the value of FDA review. The agency was able to use its EUA authorities in a flexible manner to ensure that a variety of tests reached the market and that they were accurate and reliable when used correctly. However, the agency’s regulatory authority remains unclear—a matter made more complicated by the HHS decision to limit its oversight over LDTs. As such, legislative reform is necessary to uphold FDA’s role in regulating IVDs, including those made and used in a single laboratory. Congress should pass reforms, such as those proposed by the VALID Act, to create a unified and risk-based oversight system, while also protecting the EUA powers that FDA used to increase COVID-19 testing capacity.
Endnotes
- U.S. Food and Drug Administration, “In Vitro Diagnostics EUAs,” last modified March 10, 2021, https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/vitro-diagnostics-euas.
- U.S. Food and Drug Administration, “Risk of False Results With the Curative SARS-CoV-2 Test for COVID-19: FDA Safety Communication,” Jan. 4, 2021, https://www.fda.gov/medical-devices/safety-communications/risk-false-results-curative-sars-cov-2-test-covid-19-fda-safety-communication.
- B. Melley and M. Perrone, “Congress, L.A. Take Divergent Paths After COVID Test Warning,” Associated Press, Jan. 8, 2021, https://apnews.com/article/los-angeles-california-coronavirus-pandemic-c05acb14cf888635c3e84c58eb709f70; D. Lim and S. Ferris, “Congress Using COVID Test That FDA Warns May Be Faulty,” Politico, Jan. 5, 2021, https://www.politico.com/news/2021/01/05/congress-faulty-covid-tests-fda-455099; U.S. Department of Defense, “DOD Announces Contract for 250,000 Curative Inc. COVID-19 Test Kits,” news release, July 31, 2020, https://www.defense.gov/Newsroom/Releases/Release/Article/2296901/dod-announces-contract-for-250000-curative-inc-covid-19-test-kits/; ibid.
- U.S. Department of Health and Human Services, “Rescission of Guidances and Other Informal Issuances Concerning Premarket Review of Laboratory Developed Tests,” last modified Jan. 21, 2021, https://www.hhs.gov/coronavirus/testing/recission-guidances-informal-issuances-premarket-review-lab-tests/index.html.
- L. Richardson, “Diagnostic Test Regulation Should Rank High on Agenda of New Congress,” The Pew Charitable Trusts, Jan. 11, 2021, https://www.pewtrusts.org/en/research-and-analysis/articles/2021/01/11/diagnostic-test-regulation-should-rank-high-on-agenda-of-new-congress.
- L. Richardson, “Coronavirus Pandemic Highlights Importance of FDA’s Emergency Authority,” The Pew Charitable Trusts, April 8, 2020, https://www.pewtrusts.org/en/research-and-analysis/articles/2020/04/08/coronavirus-pandemic-highlights-importance-of-fdas-emergency-authority.
- J. Shuren and T. Stenzel, “COVID-19 Molecular Diagnostic Testing—Lessons Learned,” The New England Journal of Medicine 383, no. e97 (2020), https://www.nejm.org/doi/full/10.1056/NEJMp2023830.
- U.S. Food and Drug Administration, “Coronavirus Disease 2019 Testing Basics,” last modified Nov. 6, 2020, https://www.fda.gov/consumers/consumer-updates/coronavirus-disease-2019-testing-basics.
- Ibid.
- U.S. Food and Drug Administration, “Coronavirus Disease 2019 Testing Basics”; M. Schneider et al., “From Development to Market: Understanding COVID-19 Testing and Its Challenges” (Robert J. Margolis Center for Health Policy at Duke University, 2020), https://healthpolicy.duke.edu/sites/default/files/2020-09/Margolis%20Covid%20Updated%20Sept%208.pdf.
- U.S. Food and Drug Administration, “Coronavirus Disease 2019 Testing Basics”; Schneider et al., “From Development to Market.”
- T. Parker-Pope and K.J. Wu, “What You Need to Know About Getting Tested for Coronavirus,” The New York Times, Dec. 9, 2020, https://www.nytimes.com/2020/12/09/well/live/covid-coronavirus-testing.html; R.F. Service, “The Standard Coronavirus Test, if Available, Works Well—but Can New Diagnostics Help in This Pandemic?” Science, March 22, 2020, https://www.sciencemag.org/news/2020/03/standard-coronavirus-test-if-available-works-well-can-new-diagnostics-help-pandemic.
- M. Peplow, “Rapid COVID-19 Testing Breaks Free From the Lab,” Chemical and Engineering News, Aug. 10, 2020, https://cen.acs.org/analytical-chemistry/diagnostics/Rapid-COVID-19-testing-breaks/98/web/2020/08; J. Daley, “Here’s How Coronavirus Tests Work— and Who Offers Them,” Scientific American, March 27, 2020, https://www.scientificamerican.com/article/heres-how-coronavirus-tests-work-and-who-offers-them/.
- K.J. Wu, “FDA Authorizes First At-Home Coronavirus Test,” The New York Times, Nov. 18, 2020, https://www.nytimes.com/2020/11/18/health/coronavirus-testing-home.html.
- Parker-Pope and Wu, “What You Need to Know.”
- Ibid.
- U.S. Food and Drug Administration, “Coronavirus (COVID-19) Update: FDA Authorizes Antigen Test as First Over-the-Counter Fully At-Home Diagnostic Test for COVID-19,” news release, Dec. 15, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-antigen-test-first-over-counter-fully-home-diagnostic.
- U.S. Food and Drug Administration, “Coronavirus (COVID-19) Update: FDA Authorizes First Point-of-Care Antibody Test for COVID-19,” news release, Sept. 23, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-first-point-care-antibody-test-covid-19; D.M. Hinton, chief scientist, letter to Frank Lou, director, Azure Biotech Inc., “Letter of Authorization,” Sept. 23, 2020, https://www.fda.gov/media/139789/download; Schneider et al., “From Development to Market.”
- Service, “The Standard Coronavirus Test”; Peplow, “Rapid COVID-19 Testing.”
- Parker-Pope and Wu, “What You Need to Know.”
- Ibid.
- U.S. Food and Drug Administration, “Coronavirus Disease 2019 Testing Basics”; G. Guglielmi, “The Explosion of New Coronavirus Tests That Could Help to End the Pandemic,” Nature 583 (2020): 506-09, https://www.nature.com/articles/d41586-020-02140-8.
- U.S. Food and Drug Administration, “Coronavirus Disease 2019 Testing Basics.”
- W.F. Marshall, “How Do COVID-19 Antibody Tests Differ From Diagnostic Tests?” Mayo Clinic, Dec. 12, 2020, https://www.mayoclinic.org/diseases-conditions/coronavirus/expert-answers/covid-antibody-tests/faq-20484429.
- U.S. Food and Drug Administration, “Risk of False Results.”
- U.S. Food and Drug Administration, “Coronavirus (COVID-19) Update: FDA Informs Public About Possible Accuracy Concerns With Abbott ID NOW Point-of-Care Test,” news release, May 14, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-informs-public-about-possible-accuracy-concerns-abbott-id-now-point; Abbott Diagnostics Scarborough Inc., “Fact Sheet for Healthcare Providers” (2020), https://www.fda.gov/media/136523/download.
- U.S. Food and Drug Administration, “Potential for False Positive Results With Antigen Tests for Rapid Detection of SARS-CoV-2—Letter to Clinical Laboratory Staff and Health Care Providers,” last modified Nov. 3, 2020, https://www.fda.gov/medical-devices/letters-health-care-providers/potential-false-positive-results-antigen-tests-rapid-detection-sars-cov-2-letter-clinical-laboratory.
- U.S. Food and Drug Administration, “Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Chembio Antibody Test,” news release, June 16, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chembio-antibody-test.
- T. Parker-Pope and K.J. Wu, “What You Need to Know About Getting Tested for Coronavirus,” The New York Times, Dec. 9, 2020, https://www.nytimes.com/2020/12/09/well/live/covid-coronavirus-testing.html. Out-of-pocket costs to patients, however, can range significantly—from $0 to more than $2,000, depending on their insurer and where they got the test.
- K.J. Wu, “FDA Authorizes First At-Home Coronavirus Test,” The New York Times, Nov. 18, 2020, https://www.nytimes.com/2020/11/18/health/coronavirus-testing-home.html.
- J.D. Walsh, “How Reliable Are COVID-19 Tests?” Intelligencer, June 10, 2020, https://nymag.com/intelligencer/2020/06/how-accurate-are-covid-19-tests.html; National Cancer Institute, “Sensitivity,” accessed March 11, 2021, https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/sensitivity; National Cancer Institute, “Specificity,” accessed March 11, 2021, https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/specificity.
- P. Ranganathan and R. Aggarwal, “Common Pitfalls in Statistical Analysis: Understanding the Properties of Diagnostic Tests—Part 1,” Perspectives in Clinical Research 9, no. 1 (2018): 40-43,;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5799952/.
- Ibid.
- National Cancer Institute, “PPV,” accessed March 11, 2021, https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/ppv.
- National Cancer Institute, “NPV,” accessed March 11, 2021, https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/npv.
- Ranganathan and Aggarwal, “Common Pitfalls.”
- U.S. Food and Drug Administration, “Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Chembio Antibody Test,” news release, June 16, 2020, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chembio-antibody-test.
- U.S. Department of Health and Human Services, “Rescission of Guidances.”
- Shuren and Stenzel, “COVID-19 Molecular Diagnostic Testing—Lessons Learned.”













